Chronic Kidney Disease (CKD)
Table of Contents
About chronic kidney disease (CKD)
Your kidneys do many important jobs. Some of the ways they keep your whole body in balance include:
- Removing natural waste products and extra water from your body
- Helping make red blood cells
- Balancing important minerals in your body
- Helping maintain your blood pressure
- Keeping your bones healthy
Chronic kidney disease (CKD) is when the kidneys have become damaged over time (for at least 3 months) and have a hard time doing all their important jobs. CKD also increases the risk of other health problems like heart disease and stroke. Developing CKD is usually a very slow process with very few symptoms at first. So, CKD is divided into 5 stages to help guide treatment decisions.
Signs and symptoms
Many people living with CKD do not have any symptoms until the more advanced stages and/or complications develop. If symptoms do happen, they may include:
- Foamy urine
- Urinating (peeing) more often or less often than usual
- Itchy and/or dry skin
- Feeling tired
- Nausea
- Loss of appetite
- Weight loss without trying to lose weight
People who have more advanced stages of CKD may also notice:
- Trouble concentrating
- Numbness or swelling in your arms, legs, ankles, or feet
- Achy muscles or cramping
- Shortness of breath
- Vomiting
- Trouble sleeping
- Breath smells like ammonia (also described as urine-like or “fishy”)
Causes
Risk Factors
Anyone can develop CKD - at any age. However, some people are at a higher risk than others. The most common CKD risk factors are:
- Diabetes
- High blood pressure (hypertension)
- Heart disease and/or heart failure
- Obesity
- Over the age of 60
- Family history of CKD or kidney failure
- Personal history of acute kidney injury (AKI)
- Smoking and/or use of tobacco products
For many people, CKD is not caused by just one reason. Instead, it is a result of many physical, environmental, and social factors. Early detection is important – CKD often begins without causing any noticeable symptoms. Knowing the risk factors can help you know your level of risk and if you should get checked for CKD.
Other causes
CKD can also be caused by many other conditions or circumstances. Some examples include:
- Glomerular diseases: glomerulonephritis, IgA nephropathy (IgAN), and HIV nephropathy
- Inherited conditions: polycystic kidney disease
- Autoimmune conditions: lupus (lupus nephritis)
- Severe infections: sepsis and hemolytic uremic syndrome (HUS)
- Other causes: kidney cancer, kidney stones, frequent untreated and/or long-lasting urinary tract infections (UTIs), hydronephrosis, and kidney and urinary tract abnormalities before birth
37 million adults in the United States are living with CKD - and approximately 90% do not even know they have it. Take this one-minute quiz to find out if you are at high risk for CKD.
Complications
As CKD worsens, the risk of getting complications goes up. Some examples include:
- Cardiovascular disease (heart disease and/or stroke)
- High blood pressure
- Anemia (low levels of red blood cells)
- Metabolic acidosis (buildup of acid in the blood)
- Mineral and bone disorder (when blood levels of calcium and phosphorus are out of balance leading to bone and/or heart disease)
- Hyperkalemia (high levels of potassium in the blood)
- Kidney failure
Some conditions, like cardiovascular disease and high blood pressure, can also cause or worsen CKD.
Give Today
Give today and help us provide FREE resources, support, and hope for patients, loved ones and healthcare heroes.
Diagnosis
Tests
Checking for CKD is easy with two simple tests:
- a blood test known as the estimated glomerular filtration rate (eGFR)
- a urine test known as the urine albumin-creatinine ratio (uACR)
Both tests are needed to have a clear picture of your kidney health. Having an eGFR under 60 and/or a uACR over 30 for three months or more is a sign you may have kidney disease.
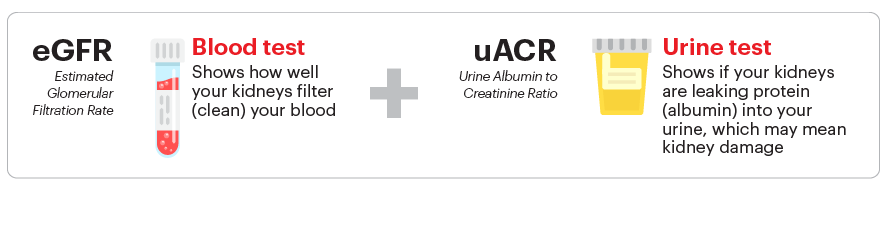
The eGFR is an estimate of how well your kidneys are removing waste products from the blood. It is calculated using your serum creatinine level, age, and sex. It can also be calculated using your cystatin C level. A “normal” eGFR varies according to age – it decreases as you get older. For this test, a higher number is better. Your eGFR number is used to determine your stage of CKD.
The uACR measures the amount of two different substances in your urine – albumin (protein) and creatinine. Healthy kidneys keep the albumin in your blood while filtering the creatinine out into the urine. So, there should be very little or no albumin in your urine. The uACR is calculated by dividing the amount of urine albumin by the amount of urine creatinine to find the ratio. For this test, a lower number is better. Your uACR number is used to test for albuminuria - a significant risk factor for complications.
In some cases, your healthcare professional may order additional tests to get more information about your kidney health. Some examples include a kidney biopsy or medical imaging (CT scan, ultrasound, or MRI).
Treatment
Overview
Managing CKD is focused on four very important goals:
- Managing the disease(s) or condition(s) that are most likely causing the CKD (for example, your diabetes, high blood pressure, or IgA nephropathy)
- Taking steps to slow down the CKD disease process directly (also known as “slowing CKD progression”)
- Lowering your risk of cardiovascular disease (having a heart attack or stroke)
- Treating any complications that you may have because of your CKD
Specific treatment recommendations depend on your stage of CKD and what other health conditions you have (including any CKD complications). Below are recommendations that apply to most people with CKD. No two people are the same, so talk with your healthcare professional about recommendations tailored to you.
Medications
Your healthcare professional may prescribe one or more medicines to help slow down or stop your CKD from getting worse. These medicines can include an ACE inhibitor/ARB, an SGLT2 inhibitor and/or an nsMRA.
Your healthcare professional may also prescribe a statin (cholesterol medicine). Guidelines recommend a statin for people with CKD who also have diabetes, a history of heart disease, or are age 50 or older. Even if you do not have high cholesterol, a statin can help lower your risk of having a heart attack or stroke.
You may also need to take additional medications or supplements to manage any CKD complications you might have (if applicable).
Nutrition
It is important to limit your sodium (salt) intake to less than 2300 mg per day (about 1 teaspoon of salt from all the food and drinks you consume each day). This recommendation is very important if you also have high blood pressure. Your healthcare professional may advise an even lower target depending on your other health conditions. This means a lot more than not using a saltshaker, but also limiting foods with high levels of sodium listed on their nutrition facts label. Some foods that don’t taste salty can have a surprising amount of sodium when you check their nutrition facts label.
Based on the results of your blood tests, your healthcare professional or kidney dietitian may also advise you to change how much potassium, phosphorus, and/or calcium you might be getting through your diet.
Meeting with a dietitian can be especially helpful if you also have other health conditions like high blood pressure, diabetes, or heart failure where it is even more important to integrate a healthy diet into your lifestyle to help prevent complications. It can feel overwhelming to keep track of so many changes, and a dietitian can help you identify what works best for you.
Additional information about eating healthy with kidney disease can be found on the Nutrition and Early Kidney Disease page.
Lifestyle recommendations
Now is a great time to make healthier lifestyle choices:
- If you smoke and/or use tobacco products, stop. Smoking can speed up the kidney disease process and increase your risk of getting kidney failure. It also increases your risk for other serious health problems, including high blood pressure, heart disease, cancers, and stroke.
- Exercise regularly. Remember, it’s okay to start slowly – taking short walks is a great way to begin.
- Sleeping well is important, too. Try to get enough sleep so you are well-rested.
- If you are overweight, losing weight through a balanced diet and physical activity can help improve your health in many ways.
- Find ways to reduce and manage stress in your life.
Other ways to lower your risk
Taking steps to manage other health conditions you may also have can also help your CKD. This includes high blood pressure, diabetes, and high cholesterol.
People with CKD should also avoid certain pain medicines known as non-steroid anti-inflammatory drugs (NSAIDs). These can be harmful to your kidneys, especially at higher doses and/or with long-term use. Some examples include:
- ibuprofen (Motrin, Advil)
- indomethacin (Indocin)
- naproxen (Aleve, Naprosyn)
- diclofenac tablets or capsules (Cataflam, Zipsor)
- celecoxib (Celebrex)
- meloxicam (Mobic)
- aspirin (only if more than 325 mg per day)
Many of these NSAID medicines are available over-the-counter (OTC) and may be sold under a different name or be mixed with other ingredients (like cough & cold medicines). Sometimes it may not be possible to avoid using these products depending on your other health conditions. Always ask your healthcare professional before using any products with these drug names or if the word “NSAID” is printed on the product’s label. In general, acetaminophen, also called Tylenol, is safe for your kidneys at recommended doses - but check with your healthcare professional first to determine the cause of your pain and the best way to treat it.
If your healthcare professional says you have metabolic acidosis, increasing the amount of fruits and vegetables you eat everyday can help lower the level of acid in your blood. This can also help slow down your CKD progression (worsening).
Preparing for your appointment
Questions to ask
- What are my eGFR and uACR numbers? What is my CKD stage?
- How high is my level of risk for developing heart disease or a stroke? What can I do to lower my risk?
- When should I have my eGFR and uACR tested again?
- Am I at a healthy weight?
- Is my blood pressure within the recommended goal range?
- Do I have diabetes or prediabetes? If so, is my A1C within the recommended goal range?
- Do I have albuminuria?
- Are there any changes I should make to my diet?
- Should I take any medication(s) to help lower my risk for CKD getting worse?
Download the NKF fact sheet: Newly diagnosed with kidney disease
- Download the NKF fact sheet: Newly diagnosed with kidney disease: English
- Download the NKF fact sheet: Newly diagnosed with kidney disease: Spanish
This content is provided for informational use only and is not intended as medical advice or as a substitute for the medical advice of a healthcare professional.