About Chronic Kidney Disease (CKD)
Your kidneys do many important jobs. Some of the ways they keep your whole body in balance include:
- Removing natural waste products and extra water from your body
- Helping make red blood cells
- Balancing important minerals in your body
- Helping maintain your blood pressure
- Keeping your bones healthy
Chronic kidney disease (CKD) is when the kidneys have become damaged over time (for at least 3 months) and have a hard time doing all their important jobs. CKD also increases the risk of other health problems like heart disease and stroke. Developing CKD is usually a very slow process with very few symptoms at first. So, CKD is divided into 5 stages to help guide treatment decisions.
Stages of CKD
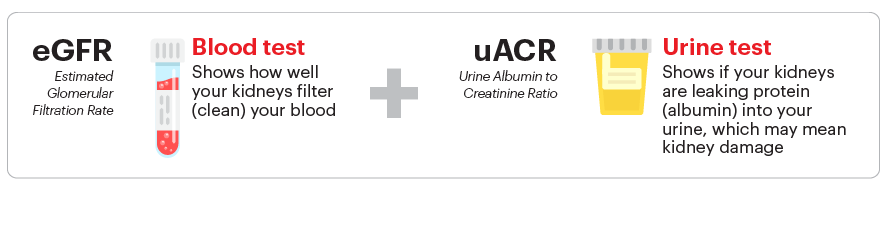
CKD is evaluated using two simple tests – a blood test known as the estimated glomerular filtration rate (eGFR) and a urine test known as the urine albumin-creatinine ratio (uACR). Both tests are needed to have a clear picture of your kidney health. When identifying your CKD stage, these tests usually need to be repeated to confirm long-term damage (lasting 3 months or more).
eGFR 90 or higher and kidney damage
(e.g. uACR 30 or higher) for 3 months or more
eGFR 60-89 and kidney damage
(e.g. uACR 30 or higher) for 3 months or more
Mild to moderate loss of kidney function
(eGFR 45-59 for 3 months or more)
Moderate to severe loss of kidney function
(eGFR 30-44 for 3 months or more)
Severe loss of kidney function
(eGFR 15-29 for 3 months or more)
Kidney failure
(eGFR less than 15 for 3 months or more)
or you are on dialysis

Help us unravel the silent threat and rewrite the future of kidney health.
- Equip patients and families with knowledge, resources, and access to high-quality care.
- Advocate for policies that address disparities and prioritize kidney health for all.
- Fund research and technology to advance early detection, improve treatment, and expand transplant access.
CKD Risk Factors
CKD Risk Factors
High blood pressure
(hypertension)
Obesity
(having a body mass index
or BMI of 30 or more)
Over the age of 60
Family history of CKD
or kidney failure
Personal history of
acute kidney injury (AKI)
Anyone can develop CKD – at any age. However, people with one or more of the risk factors above are more likely than others to develop CKD. Usually, developing CKD is not due to any single reason, but because of a combination of physical, environmental, and social factors. Early detection is important – CKD often begins without causing any obvious symptoms. Knowing the risk factors can help you know your level of risk and if you should get checked for CKD.
Take this one-minute quiz to find out if you are at high risk for CKD.
Kidney failure
Having kidney failure means that 85% to 90% of your kidney function is gone and your kidneys don't work well enough to keep you alive. There is no cure for kidney failure, but it is possible to live a long and full life with treatment. Having kidney failure is serious but with treatment, many people with kidney failure continue to have full, active lives doing things they love.
This content is provided for informational use only and is not intended as medical advice or as a substitute for the medical advice of a healthcare professional.