Table of Contents
- COVID-19 public health emergency status ending May 11
- Evusheld Loses Emergency Use Authorization
- COVID-19 public health emergency status extended
- Updates to US COVID-19 Winter Preparedness Plan
- Repeat COVID-19 infections increase the risk of hospitalization and death with each new reinfection
- During the COVID-19 pandemic, fewer people had their high blood pressure under control
- Wearing N95 face masks strongly recommended for immunocompromised people and those on dialysis
- Volunteers needed for new research on the prevention and treatment of long COVID
- Updated CDC guidance summary for a safe Halloween
- COVID-19 public health emergency status extended
- Keeping your CDC COVID-19 vaccination card up to date
- Streamlined COVID-19 guidance for people who are moderately or severely immunocompromised now available
- Breaking it down – a COVID-19 vocabulary guide
- Rebound COVID-19 infection after treatment with Paxlovid may be due to strong immune response
- While CDC streamlines COVID-19 guidance for the general public, immunocompromised people are still at high risk for severe disease
- People over age 50 may be at increased risk for shingles after recovering from COVID-19
- Bivalent COVID-19 boosters are now available and recommended
- Type 2 diabetes rates increased in young people during the COVID-19 pandemic
- Loss of smell and/or taste reported by patients with long COVID
- Moderna and Pfizer-BioNTech bivalent COVID-19 vaccines authorized for use as a booster dose
- Paxlovid is most beneficial for people over the age of 65
- Pfizer and BioNTech apply for Emergency Use Authorization of a new COVID-19 vaccine, which also protects against the Omicron variant
- Regular physical activity linked to a lower risk of COVID-19 infection and severity
- CDC recommendations for people with COVID-19 and/or those who have received a positive test result
- Vaccines reduce the risk of COVID-19 infection in patients on dialysis
- Is it time for your booster? Find out now
- COVID-19 pandemic impacted treatment decision-making for older patients with kidney disease
- Fewer people tried to quit smoking during the COVID-19 pandemic
- High blood pressure may double the risk of severe COVID, even in people who are fully vaccinated
- Smoking, vaping linked to higher risk of severe COVID-19 complications, including death
- FDA grants Paxlovid Emergency Use Authorization with certain limitations of use
- Immunocompromised people face a higher risk of hospitalization and death from COVID-19
- Omicron subvariants are surging in the US
- What if I feel sick?
- Should I get antibody testing for COVID-19?
- What is herd immunity?
- What does it mean to build up immunity?
- What should I consider if I’m on dialysis?
- What should I consider if I am planning or have undergone kidney transplant?
- Are young transplant recipients at increased risk from COVID-19?
- What can parents of young transplant recipients do?
- Am I eligible for disability benefits if I can’t work?
- What are my rights as a kidney patient if my employer wants me to return to work?
COVID-19 public health emergency status ending May 11
The first COVID-19 public health emergency was declared in January 2020, and it has been in continuous effect for almost 3 years. On January 20, 2023, the Biden Administration announced that the COVID-19 public health emergency status will end on May 11, 2023.
The end of the public health emergency means there will be changes to some of the COVID-19 government-funded programs that have been in effect since the start of the pandemic.
Key Takeaways
Now that the COVID-19 public health emergency will end on May 11, 2023, there will be changes coming. Here’s what we know so far:
- Vaccines were purchased by the government. Vaccines will continue to be available for everyone at no cost until the current supply runs out. After the supply runs out, vaccines may be covered by private and public insurance, but there may be co-pays.
- COVID-19 home tests will no longer be provided at no cost from the government. You should check with your insurance company to see if they will be covered by your policy.
- COVID-19 medication, such as Paxlovid (nirmatrelvir co-packaged with ritonavir), purchased by the government will continue to be free until the supply runs out. After the supply is gone, your medication should be covered by your insurance company and Medicare, but it will probably have a copay.
- Telehealth visits became very popular during the pandemic. Recent legislation will allow Medicare beneficiaries to continue telehealth options until December 31, 2024. Most private insurers will continue to cover telehealth after the public health emergency ends.
Evusheld Loses Emergency Use Authorization
- Evusheld is no longer authorized for emergency use due to being ineffective against new COVID-19 variants
On January 26, 2023, the US Food and Drug Administration (FDA) revised the Emergency Use Authorization (EUA) for Evusheld (tixagevimab co-packaged with cilgavimab).
Data show that Evusheld is unlikely to be effective against certain COVID-19 variants, including the main variants circulating now in the US.
Evulsheld is not currently authorized for use in the US until further notice by the Agency.
Key Takeaways
COVID-19 vaccines continue to offer the best protection against severe COVID-19. The updated booster bivalent vaccine has been reformulated with two COVID-19 strains to better protect against the most recently circulating variants. It can also help restore protection that has waned since previous vaccination. Use this tool to find out when you and others in your household can get a booster.
It is important that people who are moderately to severely immunocompromised continue to use caution, recognize the need for additional prevention measures, and remember to:
- Wear a well-fitting, high-quality N-95 mask. Properly fitting N-95 masks provide the highest level of protection.
- The CDC has a free online tool to help you find a nearby location that received N95 masks earlier this year.
- When a nearby location is found, call first to check if any free N95 masks are in stock.
- Put together your COVID-19 Personal Action Plan, so you have all the information you need on hand if you or a loved one gets sick with COVID-19.
Download, edit and save, and share your plan with your family, friends, and healthcare provider.
COVID-19 public health emergency status extended
- COVID-19 public health emergency status is extended to April 11, 2023
The first COVID-19 public health emergency was declared in January 2020. COVID-19 public health emergency declarations last 90 days and, if needed, can be extended for another 90-day period.
In the last 3 years, the emergency has been extended every time it was up for renewal. The Department of Health and Human Services has stated that it will let the public know at least 60 days before the public health emergency is lifted. With the newest extension, the COVID-19 public health emergency will last until at least April 11, 2023
Key Takeaways
Now that the COVID-19 public health emergency has been extended to April 11, 2023, you will still be able to receive COVID-19 vaccines, testing, and treatments at no cost. Medicare reimbursements for telehealth visits will also continue.
Updates to US COVID-19 Winter Preparedness Plan
- While the newer strains of COVID-19 are not as deadly as the ones seen earlier in the pandemic, the virus continues to mutate (change), and cases are on the rise
- The Federal Government is expanding the availability of free COVID-19 vaccines, tests, treatments, and masks – making them more accessible to all Americans
Winter is rapidly taking hold across the country, and COVID-19 cases are beginning to surge as more people are spending time indoors and gathering for the holidays. It’s recommended that people use at-home COVID-19 tests when they have:
- Symptoms of COVID-19
- Before and after traveling for the holidays
- Visiting indoors with immunocompromised or vulnerable people
The Biden Administration has made free COVID-19 testing widely available and easily accessible by providing:
- Over 15,000 free community testing sites nationwide
- Covering the cost of over-the-counter tests under Medicare
- Requiring all health insurance plans to cover the cost of 8 free at-home tests per month per individual, which can be easily found at local pharmacies and online
In addition, the Administration is also making COVID-19 vaccinations and treatments available to everyone in the US. This includes setting up more mobile and pop-up vaccination sites, surge testing sites, and Test-to-Treat sites where Americans can not only get tested for free but also can get safe, effective COVID-19 treatments immediately if they test positive and treatment is appropriate for them.
The Administration is also expanding access to free, high-quality N95 masks and widely distributing them through:
- Pharmacies
- Local health departments and clinics
- Aging and disability networks
- Community-based organizations
The CDC has recently launched a COVID-19 Personal Action Plan, which is an easy-to-use guide so people can make a plan including where to access free tests, the location of their closest Test to Treat site, and what to ask their provider about treatments if they test positive. The Personal Action Plan helps lay these steps out in an easy-to-use template so that all Americans – especially those at the highest risk for severe illness – can decrease their risk of getting COVID-19 and, if they become infected, have a plan to quickly seek out treatment and avoid its worst outcomes.
Key Takeaways
COVID-19 cases are rising, and the US government is providing ways to help keep Americans safer from the virus, especially those at greatest risk for developing severe illness and hospitalization. Make sure you and your loved ones are prepared with these free resources:
- Residential households in the US can order one set of 4 free at-home COVID-19 tests from the US Postal Service.
- Place your order for free at-home COVID-19 tests.
- Orders will ship free starting the week of December 19, 2022.
- Before You Throw Out "Expired" Tests: Check if your COVID-19 tests' expiration dates have been extended.
- Remember, the best way to protect yourself and others from severe COVID-19 this winter is to stay up to date on your COVID-19 vaccinations and boosters!
- Continue to wear a well-fitting, high-quality N-95 mask. Properly fitting N-95 masks provide the highest level of protection.
- The CDC has a free online tool to help you find a nearby location that received N95 masks earlier this year.
- When a nearby location is found, call first to check if any free N95 masks are in stock.
- Put together your COVID-19 Personal Action Plan, so you have all the information you need on hand if you or a loved one gets sick with COVID-19.
- Download, edit and save, and share your plan with your family, friends, and healthcare provider.
Repeat COVID-19 infections increase the risk of hospitalization and death with each new reinfection
- Study finds increased risk of severe disease leading to hospitalization and death with each reinfection after the first COVID-19 infection
- These results were found in people who had been vaccinated and boosted, as well as people who were not vaccinated
- The researchers recommend that people try to prevent a first COVID-19 infection
- In people who have already had COVID-19, the recommendation is to try to prevent reinfection
Since the COVID-19 pandemic began almost three years ago, scientists have learned that a first infection can lead to short- and long-term health risks, which can affect nearly every organ system in the body. They have also learned that people who have received vaccines and boosters, as well as people who developed antibodies from the first infection, can get COVID-19 for a second or third time.
A new study published in Nature Medicine shows how dangerous COVID-19 reinfections can be. The researchers found that repeat infections can lead to increased risk to a number of organs in the body, including the kidneys. They also found that COVID-19 reinfection leads to an increased risk of diabetes, kidney disease, and mental health issues.
In this study, the researchers analyzed about 5.8 million medical records in a database maintained by the US Department of Veterans Affairs, which is the nation’s largest combined healthcare system. Multiple ages, races, and sexes were represented, and the study participants were divided into several groups per their COVID-19 infection history. Please see the table below:
History of COVID-19 infection - March 1, 2020 to April 6, 2022 | Number of study participants |
No infection (never tested positive) | 5,334,729 |
1 infection | 443,588 |
2 infections | 37,997 |
3 infections | 2,572 |
4 or more infections | 378 |
Overall, the researchers found that people with COVID-19 reinfections were twice as likely to die and three times more likely to be hospitalized than those with no reinfection.
Also, people with repeat infections were at higher risk for developing serious COVID-19-related illnesses than those who had been infected with the virus only once – such as they were:
- 3.5 times more likely to develop lung problems
- 3 times more likely to have heart conditions
- 1.6 times more likely to experience brain conditions
Key Takeaways
Preventing COVID-19 infection is important to help lower your risk of serious disease, hospitalization, and death. Since it is almost winter, outside temperatures are getting colder and people are spending more time indoors. In addition, new variants are starting to appear, and the number of COVID-19 infections is already starting to rise in some parts of the country. People should do their best to prevent first- and repeat-COVID-19 infections. Some ways to help prevent COVID-19 infections and reinfections include:
- Staying up to date with all COVID-19 vaccinations, including all primary series doses and boosters recommended for you, when eligible.
- The people you live with or spend time with can help protect you and themselves by staying up to date on their COVID-19 vaccines too.
- Speak to your healthcare provider to see if flu and pneumonia vaccines may be appropriate for you.
- Wear a well-fitting, high-quality N-95 mask. Properly fitting N-95 masks provide the highest level of protection.
- Continue to practice social distancing and avoid poorly ventilated or crowded indoor settings.
- When indoors with others, try to improve ventilation as much as possible.
- Wash your hands often with soap and water or use a hand sanitizer that contains at least 60% alcohol.
Use the free, interactive, online tool from the CDC to find out when you or a family member can get your booster – it’s a quick and easy way to know for sure.
During the COVID-19 pandemic, fewer people had their high blood pressure under control
- Controlling high blood pressure became worse during the early months of the COVID-19 pandemic
- During this time, people with high blood pressure did not get tested as often
- When people did get their blood pressure checked, their blood pressure readings were higher than before the pandemic started
A study published in the journal Hypertension showed that during the first 8 months of the pandemic, patients with high blood pressure checked their blood pressure less often, and when they did, their blood pressure readings were higher.
The study analyzed the electronic health records of 137,593 adults with high blood pressure from 3 large healthcare systems (Cedars-Sinai/Los Angeles, Columbia University Irving Medical Center/New York City, and Ochsner Health/New Orleans). All of the participants were over the age of 18 when the pandemic began in early 2020 and had been previously diagnosed with high blood pressure.
The study found 77.8% of participants had controlled blood pressure before the pandemic. During the pandemic, the proportion of participants with controlled blood pressure decreased by 3.43 percentage points. This is concerning because even a small increase in blood pressure can put people at greater risk for heart attack, stroke, heart failure, and death.
The researchers concluded that the reasons why more people had less well-controlled high blood pressure may be due to patients:
- Not being able to get frequent blood pressure readings because doctors’ offices were closed because of lockdowns.
- Adjusting to daily life changes everyone made in 2020, such as not being as physically active, not sleeping well, unhealthy diets, increased stress, and limited access to healthcare may also have played a role.
Key Takeaways
Many people with chronic kidney disease (CKD) also have high blood pressure. Even if you do not currently have CKD, you are at high risk for developing the disease if you have high blood pressure. In fact, approximately 1 in 5 adults with high blood pressure may already have CKD – and many may not even know it. If you have high blood pressure, you should:
- Contact your doctor to take steps to manage your high blood pressure through diet and exercise or with medication.
- Check your blood pressure reading often
- Stay up to date with all your recommended vaccinations, including COVID-19 vaccinations and boosters.
Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID-19 testing after a known exposure to someone with the virus or if you are feeling ill
Wearing N95 face masks strongly recommended for immunocompromised people and those on dialysis
- People who are immunosuppressed may not be fully protected from COVID-19 infection, even if they are fully vaccinated, boosted, and are getting an Evusheld (tisagevimab/cilgavimab) shot every 6 months
- According to the CDC, Evulsheld may offer less protection against 3 strains (BA.4.6, BF.7, and BA.2.75.2) of the Omicron variant
- It is strongly recommended that people who are immunocompromised, including many who are on dialysis and kidney transplant recipients, should wear well-fitting N95 face masks
- N95 face masks are the best type of masks to help reduce the spread of COVID-19 and they offer the most protection to you and others
Wearing an N95 mask is the best way to protect yourself and others from COVID-19. Masks and respirators, when worn consistently and correctly, are effective at reducing the spread of SARS-CoV-2, the virus that causes COVID-19. N95 masks give the highest level of mask protection available at this time.
In January 2022, the federal government announced that 400 million N95 masks from the Strategic National Stockpile were available – for free – to all people living in the US. People were allowed up to 3 free masks until supplies ran out. Since that time, N95 masks have been available for people to pick up at tens of thousands of local pharmacies and health centers.
The free masks from the government were part of the response to COVID-19 surges caused by the highly contagious Omicron variant which was spreading earlier in the year and continues to circulate around the country. However, finding free N95 masks may be difficult in some areas of the US because pharmacies and health centers have limited stock at this time.
Key Takeaways
Free N95 masks were made available to the public in January 2022 and supplies may be limited.
- The CDC has a free online tool to help you find a nearby location that received N95 masks earlier this year.
- When a nearby location is found, call the pharmacy or health center to see if they still have any free N95 masks in stock.
- Ask a pharmacist or another healthcare professional, as well as a dialysis center staff member for assistance – they may be able to help you find free N95 masks.
The free N95 program is now in its 11th month, so it may be harder to find free masks. If you are unable to find any free N95 masks, they are available to buy.
- They may be available online and in some chain pharmacy locations, such as Walgreens, CVS, and Rite-Aid, as well as local independent pharmacies.
- You may also be able to find them online and in hardware stores, including Home Depot, Lowes, Ace Hardware, and Harbor Freight.
- Large chain department stores, including Walmart and Target, may also sell N95 masks both online and in stores.
- Amazon also sells N95 face masks on its website.
Learn more about N95 masks directly from two manufacturers. Visit 3M and Honeywell for more information.
For N95 masks to give you the best protection, they must be fitted correctly – which can sometimes be tricky. See this instruction sheet to make sure your N95 mask is fitting properly. The N95 instruction sheet is also available in Spanish.
Remember, it is important to use multiple prevention measures against COVID-19, including vaccines, boosters, Evulsheld, and N95 masks. Talk to a healthcare professional to find the best prevention recommendations for you.
Volunteers needed for new research on the prevention and treatment of long COVID
- Some people who have recovered from COVID-19 can experience long-term effects from their infection, known as post-COVID conditions or long COVID
- Long COVID includes a wide range of ongoing health problems; these conditions can last weeks, months, or longer
- Long COVID can also trigger other health conditions, such as diabetes or kidney disease
- Join a new research program of clinical trials to help scientists find answers for long COVID
Most people who become ill with COVID-19 start to feel better within a few days to a few weeks after infection. However, some people have long-term effects from COVID-19 infection and have symptoms that last for weeks, months, or even years. Post-COVID conditions are also known as long COVID, long-haul COVID, post-acute COVID-19, post-acute sequelae of SARS CoV-2 infection (PASC), long-term effects of COVID, and chronic COVID.
Long COVID symptoms vary from person to person and can affect almost any part of the body. Some of the symptoms people with long COVID have reported include extreme fatigue; shortness of breath; pain; difficulty sleeping; racing heart rate; not feeling up to exercise; stomach, lung, kidney, and heart issues; as well as memory and concentration problems that make it difficult to perform well at work or school.
In early 2021, the National Institutes of Health (NIH) started a research program to understand why some people do not fully recover from the virus and develop long COVID. Researching COVID to Enhance Recovery (RECOVER) is the name of the program, which includes clinical trials that are looking to find out about the long-term, ongoing health effects that some people experience after COVID-19.
RECOVER is looking for volunteers to participate in the research studies. Your experiences — whether you have long-term COVID-19 symptoms, had COVID-19 and recovered, recently tested positive for COVID-19, or never had COVID-19 — are needed.
Key Takeaways
Long COVID can be different for everyone and can affect many different parts of the body, such as the brain, heart, kidneys, and lungs. Consider volunteering for the RECOVER study. If you choose to participate in a RECOVER study:
- Researchers will ask you questions about your health, review your medical history, and monitor your health throughout the study.
- You will have check-ups with a doctor and take tests, like blood and urine (pee) tests.
- You won’t receive any treatment for long COVID as part of the study. You won’t be asked to take any medication or shots.
- You will get compensation for participating in the study.
If you would like to participate in a RECOVER study, visit this site to find a study site near you.
Updated CDC guidance summary for a safe Halloween
- On October 12, 2022, CDC recommended updated (bivalent) COVID-19 boosters for children ages 5 years and older in the United States
- The updated boosters are now available to millions of young trick or treaters – just before Halloween
It has been over 2 years now since the start of the pandemic and many people have found new ways to enjoy fall holidays, including Halloween. Seeing others in an outdoor setting is still one of the best ways to visit with friends and family and help prevent infection from COVID-19.
Luckily, it’s easy to do on Halloween because trick-or-treating usually involves plenty of outdoor time. But the holiday is not totally risk-free, which is why it is still important to be careful and do your best to prevent a COVID-19 infection.
Key Takeaways
Here are some tips for staying COVID-safe this Halloween
- Stay home if you’re sick. Skip the Halloween party if you aren’t feeling well.
- Get tested if you have COVID-19 symptoms.
- Take precautions in crowded or indoor events as informed by your county’s COVID-19 Community Level, like wearing a high-quality N-95 mask (Halloween masks don’t count). Consider making the mask part of the costume—like a doctor, nurse, ninja, or cowboy.
- If you’re hosting celebrations, review options for improving ventilation in your home. This can help you reduce virus particles in your home and keep COVID-19 from spreading.
- Keep your hands clean. If you’re out trick-or-treating, bring hand sanitizer. If you’re giving out candy, wash your hands frequently.
Remember, the best way to protect yourself and others from severe COVID-19 on Halloween (and every day) is to stay up to date on your COVID-19 vaccinations! Use this tool to find out when you and others in your household can get a booster.
COVID-19 public health emergency status extended
- COVID-19 public health emergency status is extended to January 11, 2023
In January 2020, a COVID-19 public health emergency was first declared. COVID-19 public health emergency declarations last 90 days and, if needed, can be extended for another 90-day period. Since the initial declaration in 2020, the emergency has been extended every time. The Biden administration has stated that it will let the public know at least 60 days before the public health emergency is lifted. With the newest extension, the COVID-19 public health emergency will last until at least January 11, 2023
Key Takeaways
Now that the COVID-19 public health emergency has been extended to January 11, 2023, you will still be able to receive COVID-19 vaccines, testing, and treatments at no cost. Medicare reimbursements for telehealth visits will also continue.
Keeping your CDC COVID-19 vaccination card up to date
- COVID-19 vaccination cards are updated each time you get a vaccine or booster
- Your COVID-19 vaccination card is proof of vaccination
Your COVID-19 vaccination card is a record of COVID-19 vaccinations or boosters you have received. The card is only for keeping track of COVID-19 injections and should not be confused with a vaccine record, which is also known as an immunization record. The immunization record provides a history of all the vaccines that you have received and is sometimes needed for certain jobs, traveling out of the country, and school registration.
It has been about 2 years now since COVID-19 vaccines have been available in the US. The COVID-19 card is issued by the CDC and distributed to places that administer the shots, such as pharmacies and health clinics. You cannot get a blank card directly from the CDC – they are only available from vaccine providers.
There is a place on the card for your full name and birthdate. Up to 4 vaccines and boosters can be recorded. Each line includes the product name (Moderna, Pfizer BioNTech, or Johnson & Johnson), lot number, date of the shot, and the location name where you received your shot. A vaccine provider writes in the information when you get your shot. The CDC does not record or keep track of the information that is written on your card.
Key Takeaways
Your COVID-19 vaccination card contains important medical history information and is proof that you are up to date. Please keep the following in mind:
- Bring your card to your appointment whenever you get a primary series dose or booster so that a vaccine provider can fill in information about your shot.
- You may want to take a picture of your card after each of your COVID-19 vaccination appointments so you will have a backup copy.
- When your vaccine card is full, your vaccine provider should give you another card.
- If you did not receive a CDC COVID-19 vaccination card at your first appointment, contact the vaccination provider site where you got your first shot to find out how you can get a vaccination card. You can also contact your state health department to get a copy of your vaccination record.
- Some vaccination providers and health departments may offer you access to a QR code or digital copy of your COVID-19 vaccination card in addition to giving you a physical CDC COVID-19 vaccination card. Contact your vaccination provider or local health department to learn if a digital copy of your card is available to you.
- If you were vaccinated abroad there are ways you can update your U.S. vaccination record.
- To report suspicious activity involving fake CDC COVID-19 vaccination cards, please visit Fraud Alert: COVID-19 Scams or call 1-800-HHS-TIPS.
- If you lose your card:
- Contact your vaccination provider directly to request a COVID-19 vaccination card or to get a copy of your vaccination record.
- If you cannot contact your vaccination provider site directly, contact your state health department’s immunization information system (IIS). Vaccination providers must report COVID-19 vaccinations to their IIS and related systems. Your state’s IIS cannot issue you a vaccination card, but they can provide a digital or paper copy of your vaccination record.
- If you need another COVID-19 vaccine dose and are unable to get a copy of your vaccination card or vaccination record, talk to your vaccination provider.
If you have additional questions about vaccination records, please contact your state health department. Your local or state health department can also provide more information about the laws or regulations in your area.
Streamlined COVID-19 guidance for people who are moderately or severely immunocompromised now available
- CDC has reorganized and consolidated COVID-19 vaccine and preventive information for people who are moderately or severely immunocompromised
- The new information is in an easier to read and understand format
- The US FDA continues to recommend Evusheld (tixagevimab/cilgavimab) as an appropriate option to prevent COVID-19 prior to infection, in combination with other preventive measures like getting vaccinated and boosted as recommended
- Evusheld offers protection against many of the currently circulating variants and possibly future variants
- COVID-19 vaccination schedules and guidance for people who are moderately to severely immunocompromised have not changed
The CDC has recently streamlined its guidance for COVID-19 vaccines and Evusheld, a preventive COVID-19 treatment, known as pre-exposure prophylaxis (PrEP), for people who are moderately or severely immunocompromised, including people who are kidney transplant recipients.
Please see the updated chart below:
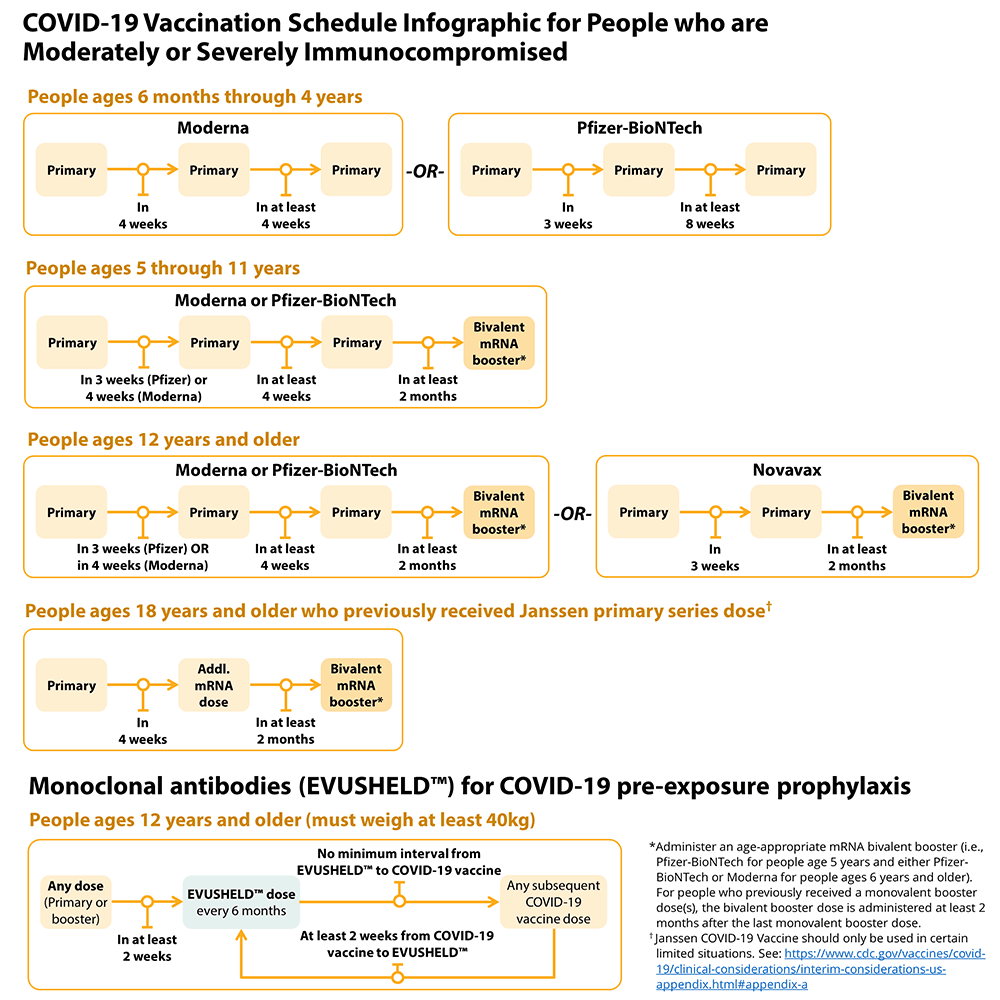
People who are or who become moderately or severely immunocompromised should follow the COVID-19 vaccination schedule according to their age and immune status at the time of eligibility for that dose. For example, people who become moderately or severely immunocompromised after completing a 2-dose mRNA primary series do not need additional primary doses; however, they should follow the schedule for people who are moderately or severely immunocompromised for the booster dose.
In addition to following the recommended COVID-19 vaccination schedule, Evusheld, a combination of two monoclonal antibodies, should be administered to people who are moderately or severely immunocompromised every 6 months for PrEP to improve the protection with the vaccine. Please remember, Evusheld is not a substitute for COVID-19 vaccination.
Key Takeaways
The current guidelines for people who are immunocompromised include:
- Staying up to date with all COVID-19 vaccinations, including all primary series doses and boosters recommended for you, when eligible.
- The people you live or spend time with can help protect you and themselves by staying up to date on their COVID-19 vaccines too.
- If your body does not have a strong enough immune response to COVID-19 vaccinations and boosters, another option is to use Evusheld, which is a medicine containing antibodies that can help prevent you from getting COVID-19.
- Even if you stay up to date on COVID-19 vaccines and receive Evusheld, taking more prevention steps can provide additional protection from getting COVID-19.
- Wear a well-fitting, high-quality N-95 mask. Properly fitting N-95 masks provide the highest level of protection.
- Continue to practice social distancing and avoid poorly ventilated or crowded indoor settings.
- When indoors with others, try to improve ventilation as much as possible.
- Wash your hands often with soap and water or use a hand sanitizer that contains at least 60% alcohol.
- Use the free, interactive, online tool from the CDC to find out when you or a family member can get your booster – it’s a quick and easy way to know for sure.
Ask your doctor, pharmacist, or other healthcare professional what’s best for you.
Breaking it down – a COVID-19 vocabulary guide
- Since the beginning of the COVID-19 pandemic, we’ve all had to learn new words related to the virus, vaccines, and treatments
- Sometimes it can be very confusing since these new words are often complex
- Here’s a quick guide to some vaccine-related words and what they mean
Primary series: Initial vaccination which can range from a single dose to a 3-dose series depending on the vaccine product and a person’s age and immune status. The same vaccine product should be used for all doses of the primary series.
Fully vaccinated: Have completed the primary series.
Additional dose: A dose of vaccine administered after the primary series to people who may be less likely to mount a protective immune response after the initial vaccination. People who are moderately or severely immunocompromised and who received Janssen COVID-19 Vaccine for their primary series are recommended to receive an additional dose using an mRNA vaccine.
Booster dose: An additional dose of vaccine administered to increase protection which might have waned over time after primary series vaccination.
- Homologous booster dose: The same vaccine manufacturer used for the booster dose and the primary series.
- Heterologous booster dose (mix-and-match booster): A different vaccine manufacturer used for the booster dose and the primary series.
Monovalent vaccine: The vaccine product is based on the original (ancestral) strain of SARS-CoV-2, the virus that causes COVID-19.
Bivalent vaccine (“updated vaccine”): The vaccine product is based on the original (ancestral) strain of SARS-CoV-2 and the Omicron BA.4 and BA.5 (BA.4/BA.5) variants of SARS-CoV-2.
Up to date: The vaccine primary series has been completed and the most recent booster dose has been administered.
Key Takeaways
Rebound COVID-19 infection after treatment with Paxlovid may be due to strong immune response
- Paxlovid (nirmatrelvir/ritonavir) is an early-stage treatment for mild-to-moderate COVID-19 in people at high risk for progression to severe disease
- COVID-19 rebound has been reported to occur between 2 and 8 days after initial recovery, with people:
- Having renewed symptoms, though usually milder than the original infection
- Testing positive for COVID-19 after having tested negative
- COVID-19 rebound occurs in people who have been treated with Paxlovid as well as those who have not
Initially, COVID-19 rebound in people who had been treated with Paxlovid was thought to be due to the drug not being strong enough to fully fight off the virus. However, findings from a small study published in Clinical Infectious Diseases suggest that COVID-19 rebound is probably not due to this cause.
In this study, the researchers wanted to better understand how COVID-19 affects white blood cells. The study included 3 separate sets of participants. Those who:
- Took Paxlovid within four days of first having COVID-19 symptoms and then had a rebound
- Did not take Paxlovid and then had a rebound
- Had COVID-19 and did not rebound
All participants were previously vaccinated and boosted against COVID-19, and none developed severe disease requiring hospitalization during the first infection or rebound. Investigators collected data on each participant’s clinical course and performed laboratory tests on blood and nasal swab samples.
The results showed that people with a rebound infection after taking Paxlovid had a very strong immune response and produced high levels of antibodies. The authors concluded that rebound symptoms are related to a strong immune response, instead of a reduced immune response.
Key Takeaways
If you test positive for COVID-19, check with your doctor to see if you may be eligible for treatment with Paxlovid. People who take a home test and are positive for COVID-19 should do the following to check if treatment with Paxlovid may be appropriate for them.
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend
- If your regular healthcare professional is not available, locate a local Test-to-Treat site, which allows state-licensed pharmacists to prescribe Paxlovid
- A call center is also available at 1-800-232-0233 (TTY 1-888-720-7489) to get help in English, Spanish, and more than 150 other languages – 8:00 am to midnight ET, 7 days a week
- The Disability Information and Access Line (DIAL) is available to specifically help people with disabilities access services. To get help, call 1-888-677-1199, Monday-Friday from 9:00 am to 8:00 pm ET or email DIAL@usaginganddisability.org
- Certain medical conditions and/or medications can have serious interactions with Paxlovid, so when you visit a pharmacy be sure to bring:
- Electronic or printed health records that are less than a year old
- A list of any prescriptions or over-the-counter medications you are taking
- Paxlovid is not recommended for patients with an estimated glomerular filtration rate (eGFR) of 30 or less
- People with an eGFR that is between 30 and 60 should be treated with a lower dose
People with an eGFR over 60 do not need any dosing changes
While CDC streamlines COVID-19 guidance for the general public, immunocompromised people are still at high risk for severe disease
- In August 2022, the CDC issued more relaxed COVID-19 guidelines for many Americans
- The revised COVID-19 guidance places greater responsibility for disease prevention on individuals
- Guidance for people who are immunosuppressed has not changed
In August 2022, the CDC released updated COVID-19 guidance. The guidance was updated because over 2 years into the pandemic, we now have more tools—vaccination, boosters, and treatments—to protect most people from getting severely ill from COVID-19.
According to the CDC, we now have a better understanding of how to prevent people from being exposed to the virus, like wearing high-quality masks, social distancing, testing, and improved ventilation indoors. The updated guidance admits that the pandemic is not over; however, Americans are trying to get to a point where COVID-19 no longer controls the daily lives of most people.
It’s important to understand, this guidance is for most people in the US. The CDC has not updated its guidance for people who are immunocompromised, which includes many people with kidney disease and kidney transplant recipients. Also, since your immune response to COVID-19 vaccination may not be as strong as in people who are not immunocompromised, there are different recommendations for COVID-19 vaccines, including boosters.
Key Takeaways
The current guidelines for people who are immunocompromised include:
- Staying up to date with all COVID-19 vaccinations, including all primary series doses and boosters recommended for you, when eligible.
- The people you live or spend time with can help protect you and themselves by staying up to date on their COVID-19 vaccines too.
- If your body does not have a strong enough immune response to COVID-19 vaccinations and boosters, another option is to use Evusheld, which is a medicine containing antibodies that can help prevent you from getting COVID-19.
- Even if you stay up to date on COVID-19 vaccines and receive Evusheld, taking more prevention steps can provide additional protection from getting COVID-19.
- Wear a well-fitting, high-quality N-95 mask. Properly fitting N-95 masks provide the highest level of protection.
- Continue to practice social distancing and avoid poorly ventilated or crowded indoor settings.
- When indoors with others, try to improve ventilation as much as possible.
- Wash your hands often with soap and water or use a hand sanitizer that contains at least 60% alcohol.
- Use the free, interactive, online tool from the CDC to find out when you or a family member can get your booster – it’s a quick and easy way to know for sure.
People over age 50 may be at increased risk for shingles after recovering from COVID-19
- Shingles is a disease that causes a painful rash
- Nearly 2 million Americans who previously had COVID-19 may be more likely to develop shingles in the six months following diagnosis
- Risk of developing shingles was higher in patients with severe cases of COVID-19 who required hospitalization
According to a new study, people aged 50 or older in the US who have had COVID-19 may be at greater risk of developing shingles compared to those who have not had COVID-19. This research was published in the Infectious Diseases Society of America’s Open Forum Infectious Diseases.
Shingles, also known as herpes zoster, is caused by the varicella zoster virus – the same virus that causes chickenpox – which becomes reactivated in the body many years after the initial infection. The disease causes a painful rash that usually occurs in a single stripe around either the left or the right side of the body and/or face. When shingles is on the face, it can affect the eyes and cause vision loss.
The study results showed that people aged 50 or older who contracted COVID-19 were 15% more likely to develop shingles compared to people who were never diagnosed with COVID-19. The risk for developing shingles was highest for up to six months after a COVID-19 diagnosis. The researchers also found that people who had been hospitalized with COVID-19 were 21% more likely to develop shingles.
Key Takeaways
Most adults over the age of 50 carry the virus that causes shingles. In people with weakened immune systems, including those with kidney disease and kidney transplant recipients, the rash may be more widespread on the body and look similar to a chickenpox rash. Please see the following for the latest CDC recommendations:
- Routine vaccination of people 50 years of age and older
- Shingrix (recombinant zoster vaccine) for the prevention of shingles and related complications.
- Two doses of Shingrix separated by 2 to 6 months for adults who are not immunocompromised aged 50 years and older.
- Vaccination of immunocompromised adults 19 years of age and older
- Shingrix for the prevention of shingles and related complications.
- The second dose of Shingrix should typically be given 2–6 months after the first.
- In people who are immunocompromised, it may be a good idea to complete the series more quickly, in which case the second dose can be given 1–2 months after the first.
Ask your doctor, pharmacist, or other healthcare professional what’s best for you.
Bivalent COVID-19 boosters are now available and recommended
- Emergency Use Authorizations (EUAs) of the bivalent Moderna COVID-19 Vaccine and Pfizer-BioNTech COVID-19 Vaccine have been authorized by the FDA and recommended by the CDC for use as a single booster dose.
- These boosters are authorized to be administered at least two months following primary or booster vaccinations.
- The Moderna COVID-19 Vaccine, Bivalent, is authorized for use as a single booster dose in individuals 18 years of age and older.
- The Pfizer-BioNTech COVID-19 Vaccine, Bivalent, is authorized for use as a single booster dose in individuals 12 years of age and older.
As has been previously reported and most already know, the virus that causes COVID-19 changes over time. The updated COVID-19 vaccine bivalent boosters include components of the original virus strain and the Omicron variant. This updated booster is called a bivalent COVID-19 vaccine booster because it is effective against two different strains of the virus
The updated COVID-19 vaccine boosters are designed to give you broad protection against COVID-19, including better protection against the Omicron variant.
As of September 8, 2022, the Centers for Disease Control and Prevention (CDC) recommends everyone stay up to date with COVID-19 vaccination, including all primary series doses and boosters for their age group:
- People ages 6 months through 4 years should get all COVID-19 primary series doses.
- People ages 5 years and older should get all primary series doses, and the booster dose recommended for them by CDC, if eligible.
- People ages 5 years to 11 years are currently recommended to get the original (monovalent) booster.
- People ages 12 years and older are recommended to receive one updated Pfizer or Moderna (bivalent) booster.
- This includes people who have received all primary series doses and people who have previously received one or more original (monovalent) boosters.
- At this time, people aged 12 years to 17 years can only receive the updated Pfizer bivalent booster.
- Getting a COVID-19 vaccine after you recover from COVID-19 infection provides added protection against COVID-19.
Key takeaways:
The CDC recently launched a free, interactive, online tool that lets you know if you are up-to-date on your COVID-19 vaccines and boosters. All you need to do is complete a quick questionnaire – no personal information is collected – and you can immediately find out if you are eligible for the new bivalent booster.
Use the new tool to find out when you or a family member can get your booster – it’s a quick and easy way to know for sure.
Reminder: COVID-19 mRNA vaccines and boosters may only offer slight protection in some immunocompromised people – if you are immunocompromised, you should:
- Check with your doctor to see if Evusheld, (tixagevimab and cilgavimab), an injectable, preventive, monoclonal-antibody medication (not a vaccine) is an appropriate prevention option for you.
- Visit the Administration for Strategic Preparedness & Response (ASPR) Therapeutic Distribution Locator to find a location near you that can provide Evusheld.
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
- Contact your doctor if you have a known exposure to someone who has COVID-19.
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend.
Remember, it is never too late to get the added protection offered by COVID-19 vaccines and boosters.
- If you need help scheduling a vaccine/booster, contact the location that set up your previous appointment
- If you need to get a vaccine/booster in a location different from where you received your previous vaccination, there are several ways you can find a vaccine provider
- There are several other ways you can look for vaccination/booster providers near you including:
- Asking your doctor, pharmacist, or community health center if they provide vaccines/boosters
- Contacting your state health department to find additional vaccination/booster locations in the area
- Checking your local pharmacy’s website to see if vaccination/booster appointments are available.
- Search vaccines.gov
- Text your ZIP code to 438829
- Call 1-800-232-0233
Type 2 diabetes rates increased in young people during the COVID-19 pandemic
- Type 2 diabetes is a disease that affects the body’s ability to control, use, and process sugar
- About 1 in 3 people under the age of 21 are at risk for type 2 diabetes due to being overweight and obese
- Young people with type 2 diabetes develop diabetes-related complications faster than those who develop type 2 diabetes as adults
- Type 2 diabetes can cause heart disease, nerve and kidney damage, vision problems, and other serious harmful medical conditions
In a multi-site study of medical records, researchers have reported a sharp rise in type 2 diabetes among children and teens during the COVID-19 pandemic. In a recent report published by The Journal of Pediatrics, the authors said this increase may be due to environmental factors.
The researchers looked at the medical records of 3,113 young patients between the ages of 8 and 21 across the United States. The average number of new type 2 diagnoses in the 2 years before the pandemic increased from 825 to 1,463 during the first year of the pandemic, which is an increase of 77%.
During the first year of the pandemic, the records showed that more boys (55%) were diagnosed with type 2 diabetes than girls (45%), which is a reverse of the percentages from pre-pandemic years. Compared with rates during the previous 2 years, the number of diagnoses in young Hispanic people almost doubled during the first year of the pandemic, and the number of diagnoses among young Black people doubled.
According to the study, the increase in type 2 diabetes diagnoses may be due to environmental factors including virtual learning for students instead of being in a classroom and the shutdown of sports and other school activities. In addition, many children and teens were less physically active because they stayed at home due to lockdowns and spent more time watching TV, playing video games, or using other electronic devices.
Key takeaways:
Until recently, young children, tweens, and teens almost never got type 2 diabetes, which is why the condition used to be called adult-onset diabetes. Now, about 33% (1 out of 3) of young people in the US are overweight or obese, which is the reason why type 2 diabetes in children and teens is rising. If your child has gained a lot of weight in the past 2 years, you should:
- Contact your child’s doctor to screen for type 2 diabetes.
- If your child already has type 2 diabetes, follow your child’s treatment plan to prevent complications, including kidney damage, due to the disease.
- Talk to your child’s doctor or other healthcare professional for recommendations about diet and exercise.
Remember, there’s a lot you can do to help your children prevent type 2 diabetes. Start by setting a new normal as a family—healthy changes become habits more easily when everyone does them together. Here are some ideas to get started:
At meals
- Drink more water and fewer sugary drinks
- Eat more fruits and vegetables
- Eat slowly—did you know it takes at least 20 minutes to start feeling full?
- Avoid eating while watching TV or using a computer
- Shop for food together
- Shop when you and your child are full, so you’re not tempted to buy unhealthy food
- Teach your child to read food labels to understand which foods are healthiest
- Have meals together as a family as often as you can
- Don’t tell your child to clean their plate
- Serve individual, small portions; let your child ask for seconds
- Reward your child with praise instead of food
Get Physical
- Aim for your child to get 60 minutes of physical activity a day, in several 10- or 15-minute sessions or all at once
- Start slow and build up
- Keep it positive—focus on progress
- Take parent-and-child fitness classes together
- Make physical activity more fun; try new things
- Ask your child which activities they like best—remember everyone is different
- Encourage your child to join a sports team
- Have a “fit kit” available—a jump rope, hand weights, resistance bands
- Limit screen time to 2 hours a day
- Plan active outings, like hiking or biking
- Take walks together
- Move more – both in-and-out of the house—activities such as, vacuuming, raking leaves, and gardening
- Turn chores into games, like racing to see how fast you can clean the house
Young kids and teens are still growing, so if your child is overweight the goal is to slow down weight gain while allowing normal growth and development. Don’t put your child on a weight loss diet without first talking to their doctor.
Loss of smell and/or taste reported by patients with long COVID
- Long COVID affects between 13% and 15% of people who have had COVID-19 and is defined as having symptoms that last longer than 3 months after COVID-19 infection
- Study finds around 30% of patients have a loss of sense of smell and/or taste, which lasts longer than 3 months
- Some patients also reported vision and hearing problems after having COVID-19
A study recently published in Frontiers in Medicine found sensory loss in people who have long COVID, with around 30% reporting a decreased sense of smell and taste lasting longer than 12 weeks after having COVID-19.
Researchers looked at the medical records of adults with long COVID symptoms, which included those with complete and partial loss of sense of smell and taste, and vision and hearing problems. Among the 4,702 people with long COVID (symptoms lasting 12 weeks or longer) included in the study:
- 31.2% -- partial loss of sense of taste
- 29.9% -- partial loss of sense of smell
- 12.2% -- complete loss of smell
- 11.7% -- complete loss of taste
Several people reported other symptoms affecting their eyes and ears, such as tinnitus (ringing or other sounds in one or both ears), blurred vision, and dry eyes.
Long COVID affects about 13% and 15% of people who test positive for COVID-19 and is defined as having COVID-19 symptoms that last longer than 12 weeks after infection. The sensory changes are generally associated with lowered quality of life, so it is very important that patients tell their doctors and healthcare professionals about their long COVID symptoms, including complete or partial loss of their sense of smell and taste, to help medical professionals advise or help manage patients appropriately.
Key takeaways:
Some COVID-19 symptoms can last for 3 months or longer. When this occurs, the condition is called long COVID. Many people with long COVID have either complete or partial loss of their sense of smell and taste. Vision and hearing problems are also a sign of long COVID. If you had COVID-19 more than 3 months ago and are still dealing with symptoms, you should contact your doctor to let them know.
Moderna and Pfizer-BioNTech bivalent COVID-19 vaccines authorized for use as a booster dose
- Emergency Use Authorizations (EUAs) of the Moderna COVID-19 Vaccine and the Pfizer-BioNTech COVID-19 Vaccine have been authorized for bivalent formulations of the vaccines for use as a single booster dose.
- These boosters are authorized to be administered at least two months following primary or booster vaccinations.
- The Moderna COVID-19 Vaccine, Bivalent, is authorized for use as a single booster dose in individuals 18 years of age and older.
- The Pfizer-BioNTech COVID-19 Vaccine, Bivalent, is authorized for use as a single booster dose in individuals 12 years of age and older.
- On September 1, 2022, the CDC issued a recommendation for the updated COVID-19 boosters from Pfizer-BioNTech and Moderna.
The virus that causes COVID-19 changes over time. The updated COVID-19 vaccine boosters include components of the original virus strain and the Omicron variant. This is called a bivalent COVID-19 vaccine because the vaccine is effective against 2 different strains of the virus.
The updated COVID-19 vaccine boosters are designed to give you broad protection against COVID-19, including better protection against the Omicron variant.
COVID-19 vaccines can help protect against severe illness, hospitalization, and death from COVID-19. As the virus changes and your immunity naturally decreases over time, you may lose some of that protection.
Key takeaways:
The FDA authorized bivalent formulations of the Moderna and Pfizer-BioNTech COVID-19 vaccines for use as a single booster dose at least two months after completing your primary or booster vaccination.
If you are eligible for an updated COVID-19 vaccine booster, the updated booster you receive does not need to be from the same manufacturer that made the vaccine you received for your primary vaccination or previous booster.
- If you need help scheduling a vaccine/booster, contact the location that set up your previous appointment
- If you need to get a vaccine/booster in a location different from where you received your previous vaccination, there are several ways you can find a vaccine provider
- There are a number of other ways you can look for vaccination/booster providers near you including:
- Asking your doctor, pharmacist, or community health center if they provide vaccines/boosters
- Contacting your state health department to find additional vaccination/booster locations in the area
- Checking your local pharmacy’s website to see if vaccination/booster appointments are available.
- Search vaccines.gov
- Text your ZIP code to 438829
- Call 1-800-232-0233
- Reminder: COVID-19 mRNA vaccines and boosters may only offer slight protection in some immunocompromised people – if you are immunocompromised, you should:
- Check with your doctor to see if Evusheld, (tixagevimab and cilgavimab), an injectable, preventive, monoclonal-antibody medication (not a vaccine) is an appropriate prevention option for you.
- Go to the Administration for Strategic Preparedness & Response (ASPR) Therapeutic Distribution Locator to find a location near you that can provide Evusheld.
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
- Contact your doctor if you have a known exposure to someone who has COVID-19.
Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend.
Paxlovid is most beneficial for people over the age of 65
- Study finds Paxlovid is most effective treating COVID-19 infection in people over 65 years of age
- In people over the age of 65, Paxlovid reduced the risk of dying by 79% and hospital admissions by 73%
- There was no evidence that treatment with Paxlovid offered any increased health benefit to people under the age of 65
According to a recent study published by The New England Journal of Medicine, early treatment with Paxlovid (nirmatrelvir/ritonavir) in people aged 65 and older reduced the risk of hospitalization and death from COVID-19
Paxlovid is an oral antiviral medication that treats symptomatic COVID-19 infection. The drug received an Emergency Use Authorization from the FDA in December 2021 and is indicated for people with symptomatic COVID-19 who are over the age of 12 and are at increased risk for having severe symptoms, hospitalization, and death.
This Israeli study looked at electronic medical records from January 9, 2022 until March 31, 2022 when the Omicron variant was the dominant COVID-19 strain in Israel and most of the world. Included in the study were people who were over the age of 40, had a confirmed diagnosis of COVID-19, and were considered to be at high risk for severe disease.
There were 109,254 patients (42,821 were over the age of 65 [39%]) whose records were reviewed for this study, including 12,662 people with kidney failure and 43,415 people who were immunosuppressed. The average age of patients was 60.
Study results showed that people, aged 65 and older, who received treatment with Paxlovid were 73% less likely to be hospitalized with severe symptoms from COVID-19 as compared to people who did not receive treatment. Their research also showed that people in this age group who were treated with Paxlovid were 79% less likely to die from COVID-19 than those who were not treated. Of note, people aged 40 to 64 did not show any significant benefit to treatment with Paxlovid.
Key takeaways:
If you test positive for COVID-19, check with your doctor to see if you may be eligible for treatment with Paxlovid, especially if you are over the age of 65. People who take a home test and are positive for COVID-19 should do the following to check if treatment with Paxlovid may be appropriate for you.
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend
- If your regular healthcare professional is not available, locate a local Test-to-Treat site, which allows state-licensed pharmacists to prescribe Paxlovid
- A call center is also available at 1-800-232-0233 (TTY 1-888-720-7489) to get help in English, Spanish, and more than 150 other languages – 8:00 am to midnight ET, 7 days a week
- The Disability Information and Access Line (DIAL) is available to specifically help people with disabilities access services. To get help, call 1-888-677-1199, Monday-Friday from 9:00 am to 8:00 pm ET or email DIAL@usaginganddisability.org
- Certain medical conditions and/or medications can have serious interactions with Paxlovid, so when you visit a pharmacy be sure to bring:
- Electronic or printed health records that are less than a year old
- A list of any prescriptions or over-the-counter medications you are taking
- Paxlovid is not recommended for patients with an estimated glomerular filtration rate (eGFR) of 30 or less
- People with an eGFR that is between 30 and 60 should be treated with a lower dose
- People with an eGFR over 60 do not need any dosing changes
Pfizer and BioNTech apply for Emergency Use Authorization of a new COVID-19 vaccine, which also protects against the Omicron variant
- Emergency Use Authorization of a booster dose of a COVID-19 Vaccine, which also includes protection from the Omicron variant, has been submitted for people who are 12 years of age and older
- The manufacturers have rapidly started production and are prepared to be ready to ship doses of the new vaccine in September 2022
The long-awaited vaccine that protects against severe illness, hospitalization, and death from COVID-19 will likely soon be available.
Pfizer and BioNTech, the manufacturers of one of the mRNA COVID-19 vaccines available in the US, recently announced they have applied for emergency use authorization of their new vaccine. Upon receiving FDA authorization, the manufacturers are ready to begin shipping doses around the country – just in time for the start of the school year and cooler autumn weather.
Large-scale studies in adults that look at the new vaccine’s effectiveness and safety have already started. Earlier studies found people who received the new vaccine were able to build a stronger immune response against the Omicron variant compared to the currently available COVID-19 mRNA vaccine.
Key takeaways:
The Pfizer-BioNTech mRNA COVID-19 vaccines have proven to be very effective in preventing severe disease, hospitalization, and death from COVID-19. In addition, these vaccines have been found to be tolerated well by most people. The vaccines are currently approved for use in people who are 6 months of age and older.
The most recent CDC recommendation is for everyone ages 6 months and older to receive the appropriate primary series of COVID-19 vaccines and also get:
- 1 Booster:
- Everyone ages 5 years and older after completing their COVID-19 vaccine primary series, if eligible
- 2 Boosters:
- Adults ages 50 years and older
- Some people ages 12 years and older who are moderately or severely immunocompromised
Remember, It is never too late to get the added protection offered by COVID-19 vaccines and boosters.
- If you need help scheduling a vaccine/booster, contact the location that set up your previous appointment
- If you need to get a vaccine/booster in a location different from where you received your previous vaccination, there are several ways you can find a vaccine provider
- There are a number of other ways you can look for vaccination/booster providers near you including:
- Asking your doctor, pharmacist, or community health center if they provide vaccines/boosters
- Contacting your state health department to find additional vaccination/booster locations in the area
- Checking your local pharmacy’s website to see if vaccination/booster appointments are available.
- Search vaccines.gov
- Text your ZIP code to 438829
- Call 1-800-232-0233
- Reminder: COVID-19 mRNA vaccines and boosters may only offer slight protection in some immunocompromised people – if you are immunocompromised, you should:
- Check with your doctor to see if Evusheld, (tixagevimab and cilgavimab), an injectable, preventive, monoclonal-antibody medication (not a vaccine) is an appropriate prevention option for you.
- Go to the Administration for Strategic Preparedness & Response (ASPR) Therapeutic Distribution Locator to find a location near you that can provide Evusheld.
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
- Contact your doctor if you have a known exposure to someone who has COVID-19.
Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend.
Regular physical activity linked to a lower risk of COVID-19 infection and severity
- Regular physical activity is linked to a lower risk of COVID-19 infection and severity, including hospital admission and death
- Physical activity of 150 minutes (2.5 hours) of moderate intensity per week or 75 minutes of vigorous intensity appears to provide the best protection
A recent study from the British Journal of Sports Medicine found that regular physical activity is associated with reduced risk of COVID-19 infection and severity of disease, as well as lower rates of hospital admission and death.
While the link between regular physical activity and COVID-19 severity is not well understood, it is thought that probably both metabolic and environmental factors are involved. The researchers wanted to better understand just how much physical activity would be needed to reduce the risks associated with COVID-19 infection, as well as hospital admission and death due to the virus.
A total of 1,853,610 adults participated in this global study and 54% were women. The average age of participants was 53.
According to the researchers, one explanation for their findings might be that regular moderate-intensity exercise may help to boost the body’s anti-inflammatory responses, as well as strengthen the heart and lungs and improve overall muscular fitness, all of which may explain its beneficial effects on COVID-19 severity.
Key takeaways:
Physical fitness is very important – especially during a pandemic. Enjoy the benefits of greater strength and feeling better since exercise keeps your body strong and healthy. With regular exercise, you may find it’s easier to get around, do your everyday tasks, and have energy left over for activities you enjoy. You may also be able to prevent infection with COVID-19 or reduce the severity of the illness should you catch the virus.
Exercise can also help with other serious diseases, including diabetes, high blood pressure, and weight problems, which are all high-risk factors for kidney disease. In addition, some of the other benefits of regular activity include:
- Improved muscle physical functioning
- Better blood pressure control
- Improved muscle strength
- Lowered level of blood fats (cholesterol and triglycerides)
- Better sleep
- Better control of body weight
Remember to speak to your doctor or healthcare professional before starting a new exercise program.
CDC recommendations for people with COVID-19 and/or those who have received a positive test result
- The Centers for Disease Control and Prevention (CDC) have released new recommendations for people who have COVID-19 and for those who have tested positive for the virus.
- Vaccines continue to offer highly effective prevention from severe COVID-19 symptoms, the need for hospitalization, and death.
On August 19, 2022, the CDC published new recommendations for people who have COVID-19 as well as for people who have tested positive, with or without symptoms, for COVID-19. The new recommendations outline the step-by-step approach you should take to protect yourself and your loved ones should someone in your household get COVID-19 and/or test positive for the virus.
See CDC Recommendations on What You Need To Know If You Have COVID-19
Key takeaways:
COVID-19 remains an ongoing public health threat; however, high levels of vaccine- and infection-induced immunity and the availability of effective treatments and prevention approaches have reduced the risk for severe illness, hospitalization, and death from COVID-19. The most recent CDC recommendation is for everyone ages 6 months and older to receive the appropriate primary series of COVID-19 vaccines and also get:
- 1 Booster:
- Everyone ages 5 years and older after completing their COVID-19 vaccine primary series, if eligible.
- 2 Boosters:
- Adults ages 50 years and older.
- Some people ages 12 years and older who are moderately or severely immunocompromised.
Remember, It is never too late to get the added protection offered by COVID-19 vaccines and boosters.
- If you need help scheduling a vaccine/booster, contact the location that set up your previous appointment
- If you need to get a vaccine/booster in a location different from where you received your previous vaccination, there are several ways you can find a vaccine provider
- There are a number of other ways you can look for vaccination/booster providers near you including:
- Asking your doctor, pharmacist, or community health center if they provide vaccines/boosters
- Contacting your state health department to find additional vaccination/booster locations in the area
- Checking your local pharmacy’s website to see if vaccination/booster appointments are available.
- Search vaccines.gov
- Text your ZIP code to 438829
- Call 1-800-232-0233
- Reminder: COVID-19 mRNA vaccines and boosters may only offer slight protection in some immunocompromised people – if you are immunocompromised, you should:
- Check with your doctor to see if Evusheld, (tixagevimab and cilgavimab), an injectable, preventive, monoclonal-antibody medication (not a vaccine) is an appropriate prevention option for you.
- Go to the Administration for Strategic Preparedness & Response (ASPR) Therapeutic Distribution Locator to find a location near you that can provide Evusheld.
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
- Contact your doctor if you have a known exposure to someone who has COVID-19.
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend.
Vaccines reduce the risk of COVID-19 infection in patients on dialysis
- Among US adults with kidney failure receiving dialysis, the risk for COVID-19 infection was highest in unvaccinated patients
- The lowest rate of COVID-19 infection was found in people who had received 3 doses of mRNA vaccine
A recent study published in the Journal of the American Society of Nephrology found that adults with kidney failure who were on dialysis were better protected from COVID-19 infection by having a third COVID-19 mRNA vaccine dose. The researchers measured patients’ antibody levels from December 25, 2021 to January 31, 2022.
Among 3,576 patients receiving dialysis, 433 patients (12%) were on a form of home dialysis and the rest received their treatment at a dialysis center. There were 901 patients (25%) who had received a third mRNA vaccine dose as of December 1, 2022, and their early antibody responses to third doses were strong.
Over the course of the study, 340 patients (7%) were found to be infected with COVID-19. The risk for infection was two times higher in unvaccinated patients and almost one and a half times higher in those patients who had received 1 or 2 doses as compared to patients who had gotten 3 doses. The highest risks for infection were in patients whose antibody levels had waned over time and in those who did not have a strong immune response to the vaccine.
Key takeaways:
Only 50% of patients on dialysis have had at least 3 mRNA vaccine doses. People who are on dialysis are at high risk for severe disease and death from COVID-19. The most recent CDC recommendation is for everyone ages 6 months and older to receive the appropriate primary series of COVID-19 vaccines and also get:
- 1 Booster:
- Everyone ages 5 years and older after completing their COVID-19 vaccine primary series, if eligible.
- 2 Boosters:
- Adults ages 50 years and older.
- Some people ages 12 years and older who are moderately or severely immunocompromised.
Remember, It is never too late to get the added protection offered by COVID-19 vaccines and boosters.
- If you need help scheduling a vaccine/booster, contact the location that set up your previous appointment.
- If you need to get a vaccine/booster in a location different from where you received your previous vaccination, there are several ways you can find a vaccine provider.
- There are a number of other ways you can look for vaccination/booster providers near you including:
- Asking your doctor, pharmacist, or community health center if they provide vaccines/boosters.
- Contacting your state health department to find additional vaccination/booster locations in the area.
- Checking your local pharmacy’s website to see if vaccination/booster appointments are available.
- Search vaccines.gov.
- Text your ZIP code to 438829.
- Call 1-800-232-0233.
- Reminder: COVID-19 mRNA vaccines and boosters may only offer slight protection in some immunocompromised people – if you are immunocompromised, you should:
- Check with your doctor to see if Evusheld, (tixagevimab and cilgavimab), an injectable, preventive, monoclonal-antibody medication (not a vaccine) is an appropriate prevention option for you.
- Go to the Administration for Strategic Preparedness & Response (ASPR) Therapeutic Distribution Locator to find a location near you that can provide Evusheld.
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
- Contact your doctor if you have a known exposure to someone who has COVID-19.
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend.
Is it time for your booster? Find out now
- Boosters are an important part of protecting yourself from getting seriously ill or dying from COVID-19
- The CDC recommends vaccines and boosters for most people including those who are moderately to severely immunocompromised
- CDC has a new easy-to-use tool to let you know if it’s time to receive a booster
The Centers for Disease Control and Prevention recently launched a free, interactive, online tool that lets you know if you are up-to-date on your COVID-19 vaccines and boosters. All you need to do is complete a quick questionnaire – no personal information is collected – and you can immediately find out if you are eligible for another vaccine dose or a booster.
Use the new tool to find out when you or a family member can get your booster – it’s a quick and easy way to know for sure.
Key takeaways:
It can be hard to keep up with the latest guidance about vaccines and boosters. The most recent CDC recommendation is for everyone ages 6 months and older to receive the appropriate primary series of COVID-19 vaccines and also get:
- 1 Booster:
- Everyone ages 5 years and older after completing their COVID-19 vaccine primary series, if eligible
- 2 Boosters:
- Adults ages 50 years and older
- Some people ages 12 years and older who are moderately or severely immunocompromised
Remember, it is never too late to get the added protection offered by COVID-19 vaccines and boosters.
- If you need help scheduling a vaccine/booster, contact the location that set up your previous appointment
- If you need to get a vaccine/booster in a location different from where you received your previous vaccination, there are several ways you can find a vaccine provider
- There are several other ways you can look for vaccination/booster providers near you including:
- Asking your doctor, pharmacist, or community health center if they provide vaccines/boosters
- Contacting your state health department to find additional vaccination/booster locations in the area
- Checking your local pharmacy’s website to see if vaccination/booster appointments are available.
- Search vaccines.gov
- Text your ZIP code to 438829
- Call 1-800-232-0233
COVID-19 pandemic impacted treatment decision-making for older patients with kidney disease
- Study looks at how the COVID-19 pandemic impacted shared decision-making between clinicians, older patients with chronic kidney disease, and their care partners
- While clinicians supported more home-based treatment plans during the COVID-19 pandemic, discussions with patients and their caregivers recommending these options were limited
COVID-19 interfered with regular medical care for many people, including older patients with advanced chronic kidney disease (CKD). A recent study published in the Clinical Journal of the American Society of Nephrology (CJASN) examined how shared decision-making—the process by which clinicians, patients, and their care partners work together to make decisions about treatments and care—was impacted by COVID-19.
In this study, researchers interviewed 76 adults (39 older patients with advanced CKD, 17 care partners, and 20 clinicians) from Boston, Portland (Maine), San Diego, and Chicago from August 2020 to December 2020. The researchers found that clinicians supported more home-based treatment plans during the COVID-19 pandemic, but actual conversations with patients and their caregivers encouraging these options were limited. Some patients reported feeling like they needed to figure out how to cope with COVID-19 and their kidney treatment options on their own.
While the early days of the COVID-19 pandemic were certainly filled with concern for many, we now have learnings that can be used moving forward. The authors of the study have stated that improvements can be made. For example, in shared decision-making during a pandemic and afterward, clinicians should consider promoting and encouraging conversations with patients who want to talk about COVID-19, with an emphasis on safety and quality of life, including the risks posed to them by COVID-19 and the impact of COVID-19 on kidney treatment options.
Key takeaways:
Some CKD treatments require outside care, for example, kidney transplants, but did you know that there are other life-saving treatments that can be done at home, such as home dialysis? In fact, in uncertain times, like a pandemic, home dialysis may, in fact, be a safer, more convenient, and less stressful option. There are a few different types to consider and discuss with your kidney doctor:
- Conventional home hemodialysis: You do this three times a week for three to four hours or longer each time. You and your care partner are trained to do dialysis safely and to handle any problems that may come up.
- Short daily home hemodialysis: This is usually done five to seven times a week using dialysis machines designed for short daily home treatments, which usually last about two hours each. Because you are doing dialysis more often, less fluid generally needs to be removed each time. This reduces symptoms like headaches, nausea, cramping, and feeling “washed out” after treatment.
- Nocturnal home hemodialysis: Long, slow treatments done at night while you sleep. You may do this kind of dialysis six nights a week or every other night. This depends on what your doctor prescribes for you. Treatments usually last about six to eight hours.
If you would like more information about home dialysis, please contact us.
Fewer people tried to quit smoking during the COVID-19 pandemic
- Smoking is a risk factor that can lead to serious diseases including diabetes, kidney disease, and heart problems
- Study finds fewer adults attempted to quit smoking since the start of the COVID-19 pandemic
- The people most affected were those who are at the highest risk for severe COVID-19 disease and other serious diseases
A recent study led by researchers at the American Cancer Society and published in the Journal of the American Medical Association (JAMA) Network Open shows that fewer adults in the US tried to quit smoking since the COVID-19 pandemic began and that these lower rates continued for over year.
The decline in the number of people who tried to stop smoking was highest for adults who are the most at risk for having severe COVID-19 and include people who self-identify as Black/African American, those with multiple health conditions or diseases, middle-aged individuals, and people with limited education.
Results from this study showed that in the past year, fewer US smokers tried to quit smoking. For the first time since 2011, the percentage of attempts to quit fell from 65.2% in 2019 to 63.2% in 2020. The decline in the number of people who tried to quit smoking started right after the beginning of the pandemic and went all the way through to early spring 2021.
According to the study, tobacco is the number one, preventable cause of cancer and is responsible for up to one-third of all cancer deaths. In addition to causing cancer, smoking can also lead to other serious diseases, including high blood pressure and diabetes, which are key risk factors for kidney disease.
Key takeaways:
To quit smoking and reduce your risk factors for serious diseases including diabetes, kidney disease, and heart problems, a combination treatment plan, using both counseling and medication, is often the best way to quit smoking for good. If you smoke, you should:
- Contact your doctor or healthcare professional for recommendations about a nearby program that may be good for you – many are available free of charge or may be covered by your health insurance plan.
- The Center for Disease Control and Prevention (CDC) has a number of programs, which are available in both English and Spanish, to help people quit smoking, including free:
- Confidential coaching through a telephone quit line, which can be reached at 1-800-QUIT-NOW (1-800-784-8669 – English) and 1-855-DÉJELO-YA (1-855-335-3569 – Spanish).
- Online resources like CDC.gov/quit and smokefree.gov.
- Texting programs you can sign up for at smokefree.gov.
- Mobile apps, such as quitSTART
The North American Quitline Consortium offers telephone and online support (information, counseling, and medication to people who want to quit using tobacco products) and serves the US, Puerto Rico, Guam, and Canada. Visit them to see information about state- and province-run programs to help you quit smoking.
High blood pressure may double the risk of severe COVID, even in people who are fully vaccinated
- Recent study finds people with high blood pressure were more than 2.5 times more likely than those who did not have high blood pressure to require hospitalization for severe COVID-19 illness.
- High blood pressure seems to be a greater risk for developing severe COVID-19 symptoms when compared with other chronic health conditions, including kidney disease, type 2 diabetes, chronic obstructive pulmonary disease (COPD), and heart failure.
According to an article published in Hypertension (an American Heart Association journal), having high blood pressure more than doubles the risk for hospitalization from an Omicron-variant COVID-19 infection – even in people who are fully vaccinated and who have received a booster dose of a COVID-19 vaccine. The study analyzed the records of adults hospitalized with COVID-19 in Los Angeles between December 2021 and April 2022.
COVID-19 vaccines helped reduce death and some of the most severe side effects from infection early in the pandemic, in particular when the Delta variant was the primary circulating variant. COVID-19 vaccine booster doses further reduced the risk of severe illness by up to 70%. Then we began to see some fully vaccinated and boosted people needing to be admitted to the hospital for severe COVID-19 symptoms during early surges of the Omicron variant at the end of 2021 and the beginning of 2022.
According to the US Centers for Disease Control and Prevention (CDC), the Omicron variant was first detected in the United States in December 2021 and continues to be the dominant variant. As of July 2022, seven Omicron subvariants have been identified.
This study looked at 912 adults who had received at least 3 doses of an mRNA COVID-19 vaccine (Pfizer-BioNTech or Moderna) and were treated for COVID-19 during an Omicron surge, between December 2021 and April 2022, in the greater Los Angeles area. Demographic information, including age, gender, race, ethnicity, and clinical data from electronic health records, were also examined. Scientists identified and analyzed a number of other factors including chronic health conditions, such as type 2 diabetes, kidney disease, heart attack, heart failure, and prior chronic pulmonary obstructive disease (COPD) or asthma.
The researchers found:
- Of the 912 adults who received three doses of an mRNA COVID-19 vaccine, nearly 16% required hospitalization.
- Older age, high blood pressure, chronic kidney disease, heart attack, heart failure, and the time between the last vaccination and COVID-19 infection were all associated with a greater need for hospitalization.
- People with high blood pressure were 2.6 times more likely to require hospital care for severe COVID-19 illness, even when the patient had no other serious chronic health condition
- Of the 145 patients hospitalized, 125 of them (86.2%) had high blood pressure
Key takeaways:
Many people with kidney disease also have high blood pressure. Even if you do not currently have kidney disease, you are at high risk for developing kidney disease if you have high blood pressure. In fact, approximately 1 in 5 adults with high blood pressure may already have chronic kidney disease – and many may not even know it. If you have high blood pressure, you should:
- Contact your doctor to take steps to manage your high blood pressure through diet and exercise or with medication.
- Stay up-to-date with all your recommended vaccinations, including COVID-19 vaccinations and boosters.
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
- Contact your doctor if you have a known exposure to someone who has COVID-19
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend
Smoking, vaping linked to higher risk of severe COVID-19 complications, including death
- People who smoke or vape were 45% more likely to die and 39% more likely to receive mechanical ventilation when compared with those who did not smoke or vape.
- Although the excessive risk due to smoking was independent of medical history and medication use, smoking was a stronger risk factor for adults between the ages of 18 and 59 years.
People who said they had smoked or vaped prior to their hospitalization for COVID-19 were more likely than other people who did not smoke or vape to experience severe complications, including death, from COVID-19 infection. The findings are from a recent study based on data from the American Heart Association’s COVID-19 CVD Registry and published in PLOS ONE, a peer-reviewed, open-access scientific journal published by the Public Library of Science.
Researchers looked at records from adults who were hospitalized with COVID-19 in 107 US hospitals between January 2020 to March 2021. Smoking status was self-reported and people were classified as smokers if they reported currently using either traditional, combustible cigarettes or e-cigarette products. The analysis reviewed records for a total of 4,086 people, comparing 1,362 people who smoked or vaped to 2,724 people who did not smoke or vape. There was no statistically significant difference in age, sex, race, medical history, or medication between the two groups.
The study found that people who smoke or vape tend to have a higher risk of developing health conditions, such as obesity and high blood pressure, which are also known risk factors for serious diseases including diabetes, kidney disease, chronic obstructive pulmonary disease (COPD), and heart problems that could lead to severe COVID-19 illness and death.
Key takeaways:
Smoking is a risk factor that can lead to serious diseases including diabetes, kidney disease, chronic obstructive pulmonary disease (COPD), and heart problems. If you smoke or vape you should:
- Contact your doctor and look into ways that you quit
- More to come (smoking cessation programs, websites, numbers)
- Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
FDA grants Paxlovid Emergency Use Authorization with certain limitations of use
Paxlovid is an oral antiviral drug that must be taken within 5 days after COVID-19 symptoms begin
Paxlovid is NOT authorized to treat patients who are:
Hospitalized due to severe or critical COVID-19
Seeking either pre-exposure or post-exposure prevention of COVID-19
On treatment with Paxlovid for more than 5 consecutive days
Currently, Paxlovid is not FDA-approved to prevent or treat any diseases or conditions, including COVID-19 – it is an investigational drug that has received FDA Emergency Use Authorization
Paxlovid is not recommended for patients with an eGFR of 30 or less
The US Food and Drug Administration (FDA) recently revised the Emergency Use Authorization (EUA) for Paxlovid (nirmatrelvir and ritonavir). Paxlovid has received an EUA for the treatment of mild-to-moderate COVID-19 in adults and children 12 years of age and older who weigh approximately 88 pounds or more. Eligible patients include those who test positive for COVID-19 and are at high risk of severe illness, including hospitalization or death. Paxlovid must be taken within five days after COVID-19 symptoms begin. On July 6, 2022, the FDA announced the authorization of state-licensed pharmacists to prescribe Paxlovid to eligible patients to expand access to those who have recently become ill with COVID-19.
Key takeaways:
If you test positive for COVID-19, check with your doctor to see if you may be eligible for treatment with Paxlovid. People who take a home test and are positive for COVID-19 should do the following to check if treatment with Paxlovid may be appropriate for you.
- Contact your doctor if you test positive for COVID-19 and take any medications for COVID-19 that your doctor may recommend
- If your regular healthcare professional is not available, locate a local Test-to-Treat site, which allows state-licensed pharmacists to prescribe Paxlovid
- A call center is also available at 1-800-232-0233 (TTY 1-888-720-7489) to get help in English, Spanish, and more than 150 other languages – 8:00 am to midnight ET, 7 days a week
- The Disability Information and Access Line (DIAL) is available to specifically help people with disabilities access services. To get help, call 1-888-677-1199, Monday-Friday from 9:00 am to 8:00 pm ET or email DIAL@usaginganddisability.org
- Certain medical conditions and/or medications can have serious interactions with Paxlovid, so when you visit a pharmacy be sure to bring:
- Electronic or printed health records that are less than a year old
- A list of any prescriptions or over-the-counter medications you are taking
- Paxlovid is not recommended for patients with an estimated glomerular filtration rate (eGFR) of 30 or less
- People with an eGFR that is between 30 and 60 should be treated with a lower dose
- People with an eGFR over 60 do not need any dosing changes
Immunocompromised people face a higher risk of hospitalization and death from COVID-19
Study finds a link between people who are immunocompromised and their increased risk of intensive care unit (ICU) admission and death from COVID-19 infection.
22,345 vaccinated and unvaccinated patients in 10 states participated in the study.
3,391 study participants had kidney disease, 353 had received a solid organ transplant, and 610 were taking steroids.
The Centers for Disease Control and Prevention (CDC) released a report on July 8, 2022, which shows that vaccinated and unvaccinated immunocompromised patients accounted for 12.2% of all adult COVID-19 hospitalizations in 10 states.* The study also found that immunocompromised patients have a greater likelihood of both being admitted to the ICU and death due to COVID-19 infection than those who are not immunocompromised.
* States include California, Colorado, Connecticut, Georgia, Michigan, Minnesota, New Mexico, New York, Oregon, and Tennessee.
Key takeaways:
Immunocompromised people are at increased risk for severe COVID-19 infection and illness and should continue to try to prevent exposure to COVID-19. Recommended approaches include:
Wearing an N95 mask and social distancing when indoors with people who do not live in your household
Being up to date on all COVID-19 vaccinations and boosters
Contacting your doctor if you have a known exposure to someone who has COVID-19
Contacting your doctor if you test positive for COVID-19 and taking any medications for COVID-19 that your doctor may recommend
Omicron subvariants are surging in the US
BA.4 and BA.5 – subvariants of the Omicron variant – now make up 80% of COVID-19 cases in the US with BA.5 accounting for most of the cases
These omicron variants appear to spread more easily than other variants
Early reports suggest that the BA.5 subvariant may be more likely to escape immunity from prior COVID-19 infections, as well as COVID-19 vaccines and boosters
COVID-19 vaccines and boosters also provide less immune protection from the BA.5 subvariant, especially since fewer people are up to date on their vaccinations and boosters, leading to waning immunity
More than 222 million Americans are fully vaccinated against COVID-19, over 106 million people have at least their first booster shot, and just about everyone living in the US is eligible for vaccination. In addition, there are now more lifesaving treatments that are readily available, as well as low-cost and free government-provided at-home tests, and high-quality N-95 masks. Based on the latest Centers for Disease Control and Prevention, (CDC) data, adults who are up to date with their vaccinations are 3.5 times less likely to be hospitalized than unvaccinated adults who are 50 years of age and older. People who have received two booster shots are 42 times less likely to die from COVID-19 compared to those who are unvaccinated. Vaccines are free and easy to get at 90,000 convenient locations nationwide. The guidance is clear that every American, age 5 and over, should receive a booster five months after their primary series, and people age 50 and older or those who are moderately or severely immunocompromised should receive a second booster shot at least four months after their first.
Key takeaways:
As Omicron subvariant BA.5 cases continue to rise, the US government will continue to provide support to people who are immunocompromised.
Continue to practice good prevention habits, including wearing N95 masks when in public, social distancing, and COVID testing after a known exposure to someone with the virus or if you are feeling ill.
Make sure you are up to date on all recommended vaccines
Contact your doctor if you test positive for COVID-19 or locate a local Test-to-Treat site
A call center is also available at 1-800-232-0233 (TTY 1-888-720-7489) to get help in English, Spanish, and more than 150 other languages – 8:00 am to midnight ET, 7 days a week
The Disability Information and Access Line (DIAL) is available to specifically help people with disabilities access services. To get help, call 1-888-677-1199, Monday-Friday from 9:00 am to 8:00 pm ET or email DIAL@usaginganddisability.org
Certain medical conditions and/or medications can have serious interactions with antiviral treatments, so when you visit a pharmacy be sure to bring:
Electronic or printed health records that are less than a year old
A list of any prescriptions or over-the-counter medications you are taking
What if I feel sick?
If you feel sick, follow these steps:
- Stay home except to get medical care (including dialysis treatments)
- Do not go to work or school
- Contact and follow the advice of your healthcare provider
- Separate yourself from other people
- Watch your symptoms
If you have a fever, cough or other symptoms you might have COVID-19. Other COVID-19 symptoms may include chills, muscle pain, headache, sore throat, or new loss of taste or smell. Emergency warning signs include trouble breathing, persistent pain or pressure in the chest, new confusion or inability to arouse, bluish lips or face.
You can find more information about what to do if you feel sick on the Centers for Disease Control (CDC) website.
Should I get antibody testing for COVID-19?
You can ask your healthcare team, or check with local/state health departments, to help decide if you should receive an antibody test and if it can be done safely for people with kidney disease.
Serological tests detect antibodies in the blood when the body is responding to a specific infection, such as COVID-19. They are also known as antibody tests. These antibodies are produced when someone has been infected, so a positive result from this test indicates that person was previously infected with the virus.
Antibody tests can help clinicians and their patients find out if someone was previously infected with COVID-19. The information can help researchers figure out how much the virus has spread in a community and to see if people can donate convalescent plasma, which might help others sickened by COVID-19. However, research is ongoing to see if antibodies from a CVOID-19 infection can protect someone from reinfection and if this protection lasts.
Also, these tests can have limitations. For example, specificity (doesn’t detect non-target viruses) and sensitivity (true positive rate, meaning antibodies exist) of antibody tests may vary. The CDC is evaluating the performance of antibody tests in collaboration with the FDA and other federal organizations.
State and Territorial Health Departments
What is herd immunity?
The CDC defines herd immunity as “protection from disease in a group, due to a large enough proportion of the population having immunity to prevent the disease from spreading from person to person.”
The idea is that if a large enough portion of a population is immune to a certain infection (either through recovery or vaccination) then transmission would slow and serve as a barrier for others without immunity.
However, a very large portion of the population would need to be immune to an infectious disease, such as COVID-19. People who have recovered from an infection may be protected from reinfection for a time, based on what is known about other viruses (research is ongoing). However, many, many more people would need to be infected for this to possibly work, which would mean many more people would get sick and possibly die. This is why general recommendations and strategies have focused on social distancing (such as maintaining a distance of 6 feet from others).
What does it mean to build up immunity?
The immune system is the body's defense against infections. Part of this defense involves making antibodies to help keep the body protected from future infections. An antibody is made to protect against a certain virus or other germ.
It’s possible to build up protection or immunity by antibodies produced from an infection, such as with COVID-19, based on what is known about other viruses. However, this is a new virus and research is ongoing to see if antibodies from a COVID-19 infection can protect someone from reinfection and if this protection lasts.
What should I consider if I’m on dialysis?
First and foremost, you should know that you are still at increased risk for infection and for worse complications if you catch COVID-19.
Please keep in close contact with your dialysis center for any further recommendations or instructions.
Visit the CDC for more information.
What should I consider if I am planning or have undergone kidney transplant?
People who plan to or have already had a kidney transplant are at increased risk of developing severe illness from COVID-19 and preventing your exposure to the virus is the best approach.
Please keep in close contact with your transplant center for any further recommendations or instructions
Visit the CDC for more information.
Are young transplant recipients at increased risk from COVID-19?
Since the start of the pandemic, most of the children admitted to pediatric intensive care units with severe COVID-19 symptoms have underlying conditions, such as kidney transplant recipients who are immunosuppressant medication.
Also concerning, a growing number of children have been identified who appear to have a different response to COVID-19, which doctors have called Pediatric Multi-System Inflammatory Syndrome. The symptoms of Pediatric Multi-System Inflammatory Syndrome include a persistent fever, rash, as well as gastrointestinal symptoms such as vomiting and diarrhea. Young patients can also suffer from cardiac inflammation.
What can parents of young transplant recipients do?
The best way to keep children on immunosuppressant treatment well is to prevent their exposure to the virus. Continue to practice everyday preventive actions to help reduce your risk of getting sick and infecting your child and
- Avoid close contact with people who are sick
- Stay home when you are sick, except to get medical care
- Cover your coughs and sneezes with a tissue and throw the tissue in the trash
- Wash your hands often with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing; going to the bathroom; and before eating or preparing food
- Use an alcohol-based hand sanitizer with at least 60% alcohol, if you’re unable to wash your hands (eg, using a gas pump)
- Clean and disinfect frequently touched surfaces and objects (eg, tables, countertops, light switches, doorknobs, and cabinet handles)
Contact your child’s transplant center for more information.
[rating_widget|what-parents-young-transplant-recipients-can-do]
Am I eligible for disability benefits if I can’t work?
It is possible that you are eligible for disability benefits if you can't work due to COVID-19. Your social worker can give you information about financial programs, what the qualifications are, and how to apply.
The federal government runs 2 of the best-known programs.
- Social Security Disability Insurance (SSDI) is a program of the Social Security Administration (SSA). It pays a monthly cash benefit to people who are unable to work for a year or more because of a disability.
- Supplemental Security Income (SSI) is another SSA program. Benefits are calculated based on an individual’s financial needs, not the amount of tax that they paid. SSI pays its benefits monthly. This amount may be supplemented by state or local benefits.
What are my rights as a kidney patient if my employer wants me to return to work?
There are laws to protect people with chronic conditions and illnesses from discrimination in the workplace. Your legal rights may be protected by one of the following federal acts.
Americans with Disabilities Act (ADA)
If you work for a company with 15 or more employees, the Americans with Disabilities Act (ADA) requires your employer to make any “reasonable accommodations” that you might need in order to perform your work duties.
Examples include:
- Making parking lots, bathrooms, and work areas handicapped accessible
- Allowing you to work from home if possible, in your current role
- Having flexible work schedules (to schedule around dialysis treatments for example)
- Designating a sterile area to exchange cleansing fluid bags for PD
- Reassigning you to a less strenuous job if you request one and one is available
- Assigning any of your non-essential tasks to other employees, at your request
The Equal Employment Opportunity Commission (EEOC) handles complaints under the ADA.
Family and Medical Leave Act (FMLA)
If you work at least 20 weeks of the year for an employer with 50 or more employees, you may qualify for the Family and Medical Leave Act (FMLA). The FMLA allows for 12 weeks of unpaid, job-protected leave for medical reasons.
If you had group health insurance coverage before taking leave, it will continue under the same terms or conditions.
Your employer can ask for medical certification stating that you have a serious illness but cannot punish you for taking leave to have surgery or begin treatment. Your spouse, children, or parents may also be eligible for FMLA leave if you need them to provide you with care or transportation.
The Department of Labor (DOL) handles complaints under FMLA.