About the Initiative
Chronic Kidney Disease (CKD) is a major public health issue that is underrecognized, underdiagnosed, and sees longstanding health disparities that disproportionately impact BIPOC, LGBTQIA+, undocumented, and other disinvested communities. Of the estimated 4.4 million adults in California living with CKD, 3.960 million are unaware of their diagnosis. Meanwhile, about 22% of Californians at-risk1 for CKD are being properly tested.
Recognizing that a community-based, multi-dimensional approach is necessary to overcome these challenges, the National Kidney Foundation is advancing a Collective Impact strategy to develop and advance equitable solutions to improve CKD testing and diagnosis in primary care. These Ending Disparities in CKD Leadership Summits will convene stakeholders to participate in a series of “Learning and Action Workgroup” meetings.
We hosted a Bay Area Ending Disparities in CKD Leadership Summit in March 2024, and a Southern California Summit in June 2025. To learn more about each Summit, please visit the individual pages below:
1 “At-risk” is defined as having diabetes, hypertension, or both.
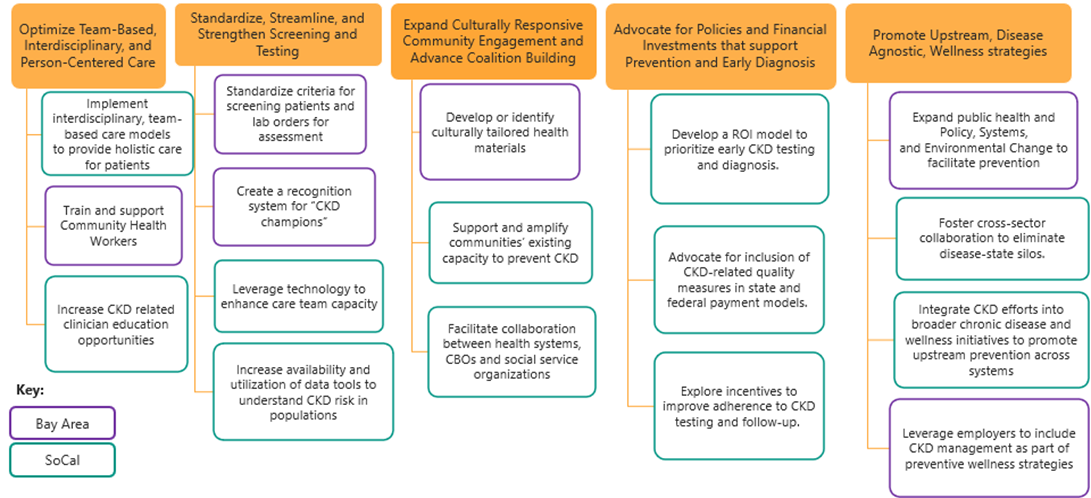
California Roadmap
Following our Bay Area Summit in 2024 and Southern California Summit in 2025, we identified an opportunity to develop a California-wide implementation strategy—one that builds on regional insights while addressing the state’s broader and diverse needs.
While both regions provide valuable perspectives, we know they do not reflect the full range of experiences and unique needs across California. This is an evolving, collaborative effort, and we’re committed to advancing CKD prevention and care for all Californians.
Explore our statewide roadmap below, and check back here for implementation updates.
Land Acknowledgement
While we refer to the state of California, we acknowledge that this land stands upon the ancestral and unceded territories of 109 federally recognized tribes and numerous non-federally recognized tribes petitioning for recognition. We recognize both the historical and ongoing injustices experienced by Indigenous communities—including the impacts of settler-colonization and genocide—as well as their resilience, achievements, and leadership.
In the spirit of continuous learning and accountability, we humbly offer the following resources for further exploration:
- Native Land Digital
- State of California: Native American Heritage Commission
- Southern California Tribal Chairmen's Association
- County of Los Angeles: Land Acknowledgement
- Sogorea Te’ Land Trust
- The Association of Ramaytush Ohlone
- San Francisco State University’s American Indian Studies Department
- UCSF Land Acknowledgement and Resource
Roadmap Implementation
Disseminate NKF's CKD patient education to individuals with risk factors
In partnership with the Alameda County Community Food Bank (ACCFB), we developed an education resource (in English and Spanish) on CKD for patients who are living with diabetes. This flyer will be included in the medically tailored food boxes that ACCFB provides through CalAIM. We look forward to evaluating this pilot and are grateful to ACCFB for their partnership! We welcome additional community nutrition partners to join this initiative.
Train Community Health Workers (CHW) and Patient Navigators
According to the National Center for Farmworker Health, common diagnoses among agricultural workers include obesity, diabetes, and hypertension, all of which are risk-factors for CKD. With one third to half of all agricultural workers in the US residing in CA, we are seeking funding to tailor and deploy the NKF's CHW training modules to better support those CHWs who work with this population.
Sources:
- NCFH. A Profile of Migrant Health: 2022 Analysis of HRSA Health Center Data.
- NCFH. Farm Labor Data Dashboard. Date Accessed: 06 August 2024. https://ncfh.org/dashboard.html.
Leverage team-based care models to provide holistic care for patients
The NKF CNOW (CA, NV, OR, WA) team hosted a pilot presentation on co-management at our Journal Club. Brian Brady, MD--one of our Summit partners--and Jo-Anne Suffoletto, MD from Stanford University presented on Partnering with Primary Care and Considering Non-Steroidal MRAs in the Chronic Kidney Disease Treatment Armamentarium. Watch the recording here.
We are seeking partners to implement similar workshops throughout our CNOW region. Contact nina.sherpapine@kidney.org if you'd like to learn more!
Develop shared messaging and health promotion or wellness programs
To better identify shared messaging opportunities on chronic disease, we are participating in local health promotion and wellness coalitions. We participated in the California Department of Public Health's Healthy Hearts California Learning Collaborative and will be joining the San Francisco Department of Public Health's Shape Up San Francisco Coalition. We are also seeking opportunities to support additional chronic disease prevention coalitions or collaborate on health promotion activities.
The NKF CKDintercept team has developed a Public Health Professional CKD Educational Toolkit, which empowers public health professionals to enhance CKD awareness and its interconnectedness with cardiovascular disease outcomes.
Improve primary care workflows and tools to support testing and management.
We are connecting with health systems across the Bay Area to engage in the NKF's Data Strategy and Learning Collaborative. These resources have helped other institutions improve guideline concordant testing by as much as 60%. Contact mallory.caron@kidney.org if you'd like to learn more!
Summit partner, Delphine Tuot, MD, is supporting Oregon Community Health Information Network and the San Francisco Community Clinic Consortium in leveraging Epic to increase uACR testing for patients with hypertension.
We are collaborating with the Purchaser Business Group on Health's California Quality Collaborative on technical assistance for a payment model demonstration project by providing our CKD Change Package resources.
Ways to Get Involved
The NKF is committed to advancing population health initiatives focused on CKD and chronic disease prevention, and prioritizing the well-being of our communities. Achieving sustainable system change requires careful planning, collaboration, and time—and we need your support!
If you're interested in partnering on any of the recommendations currently in progress or other ideas, please reach out to us. Thank you for your commitment to this vital work!
- Nina Sherpa-Pine (she/her/hers/any pronouns used respectfully), Director of Community Impact and Health Partnerships: nina.sherpapine@kidney.org
- Mallory Caron (she/her/hers), Senior Manager Population Health Partnerships: mallory.caron@kidney.org