Last updated: July 23, 2025
Medically reviewed by: NKF Patient Education Team
Hyperkalemia is high potassium in the blood, often caused by kidney disease. Symptoms include muscle weakness and heart issues. Treatment can include medication and diet changes.
About High Potassium
High potassium (called “hyperkalemia”) is a medical problem in which you have too much potassium in your blood. Your body needs potassium. It is an important nutrient that is found in many of the foods you eat. Potassium helps your nerves and muscles, including your heart, work the right way. But too much potassium in your blood can be dangerous. It can cause serious heart problems.
Signs and Symptoms
Many people have few, if any, symptoms. If symptoms do appear, they are usually mild and non-specific. You may feel some muscle weakness, numbness, tingling, nausea, or other unusual feelings. It usually develops slowly over many weeks or months and is often mild. It can come and go.
If high potassium comes on suddenly and you have very high levels of potassium, you may feel heart palpitations (very fast or pounding heart beats in your chest), shortness of breath, chest pain, nausea, or vomiting. Sudden or severe hyperkalemia is a life-threatening condition. It requires immediate medical care.
High Potassium and Kidney Disease
High potassium is common in people with kidney disease, especially when it is advanced. Healthy kidneys control the right amount of potassium in your blood. Potassium is taken in through the foods you eat and the liquids you drink. It is filtered by the kidneys and lost through the urine. In the early stages of kidney disease, the kidneys can often make up for high potassium.
However, high potassium can happen if your kidneys do not work well. When kidneys do not work as well as they should, the amount of potassium in the blood can increase. It is the job of the kidneys to balance the amount of potassium taken in with the amount lost in urine. But as kidney function gets worse, they may not be able to remove enough potassium from your body.
Causes
High potassium can have many causes. Some factors, such as certain medicines and supplements, become more of an issue with certain diseases, such as advanced kidney disease. Some causes may include, but are not limited to the following:
- Certain medicines, dietary supplements, and dialysate prescriptions: Some medications or supplements might have potassium and directly raise blood potassium levels. Other drugs do not have potassium, but indirectly cause higher potassium in the blood. For people on dialysis, the potassium in your dialysate may be too high and your doctor may need to lower it.
- Salt substitutes: Many salt substitutes contain high amounts of potassium in the form of potassium chloride instead of sodium chloride (table salt).
- Certain foods or drinks in large amounts: Certain food and drinks have higher levels of potassium. Usually, the body can handle the excess potassium, but people with kidney disease, especially when it’s more advanced, may not be able to remove excess potassium.
- Other diseases: Diabetes, heart disease, kidney disease and other diseases can lead to higher blood potassium. Diabetes and heart disease can damage kidneys, leading to high potassium. Damaged kidneys are less able to remove the excess potassium from the blood. Certain hormones can also play a role with some diseases. For example, insulin deficiency in diabetes can raise potassium levels in the blood by blocking potassium from entering cells. Aldosterone is a hormone that regulates sodium and potassium balance in the kidneys. With heart failure, levels of aldosterone can be higher, which can reduce potassium excretion from the body. This raises blood potassium levels.
Diagnosis
A simple blood test is used to measure the level of potassium in your blood. If you are at risk of high potassium, be sure you ask your healthcare professional about checking your potassium level.
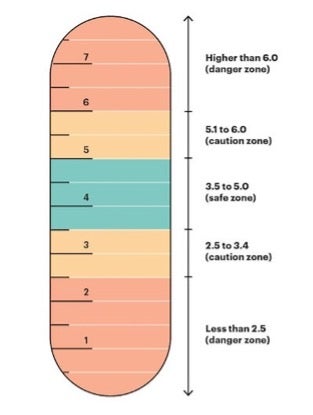
For most healthy people, the level of potassium in the blood should be between 3.5 and 5.0, depending on the laboratory that is used. High potassium is usually defined as a blood potassium level above 5.0. While slight increases in potassium usually does not show any symptoms, high potassium levels may cause life-threatening heart problems, muscle weakness, or paralysis. Symptoms usually happen at levels higher than 6.0. However, the speed of potassium increase can be more impactful than the number itself. Also, some people may have a higher potassium level and not feel any symptoms, while others may feel symptoms at a lower potassium level. This is why it is important to get regular checkups and report any problems to your healthcare team.
It should be noted that low potassium, a condition known as hypokalemia, can also be very serious (below 3.5). Hypokalemia also needs to be tested for and treated. It is important to have the right amount of blood potassium.
Treatment
Overview
Treatment of high potassium can include medicine or dietary changes. Your healthcare professional will also look for causes of high potassium. You will be asked about your medical history, your diet, and the medicines you take. This will help determine what caused your high potassium and plan your treatment.
It is important that you tell your healthcare professional about all the medicines you take, even over-the-counter products such as herbals and other supplements. Some medicines might raise potassium. Your healthcare professional will tell you if any changes in your medicines are needed. Do not stop taking medicine unless a healthcare professional tells you to do so.
Medications
Certain medicines might be used to treat high potassium.
- Potassium binders often come in the form of a powder. They are mixed with a small amount of water. When swallowed, they can attach or “bind” to extra potassium in your intestines and remove it.
- Diuretics, or water pills, help rid your body of extra potassium. They work by making your kidney create more urine. Potassium is normally removed through urine. Diuretics may not work well when kidney function is low.
Nutrition
Fruits, vegetables, nuts and legumes, although high in potassium, are part of a healthy diet in kidney disease. If medicine or other changes in medical care don’t lower your potassium, then some foods may need to be limited.
Even people who need to limit potassium should eat plenty of fruits and vegetables. Less potassium is absorbed from plant foods, and their fiber content may improve constipation and increase potassium excretion. They can also improve acidosis and are linked to a slower progression of kidney disease. You may be asked to follow a lower-potassium diet if higher potassium levels remain an issue. Avoid certain salt substitutes. These can be high in potassium. Also avoid foods that have potassium additives like potassium sorbate. Having too much potassium can be harmful, but having too little can cause problems, too. A kidney dietitian can create a meal plan that’s right for you.
