Last updated: July 06, 2023
Medically reviewed by: NKF Patient Education Team
Stage 4 CKD means severe kidney function loss. Symptoms include fatigue, swelling, and nausea. Regular check-ups and lifestyle changes are crucial for managing it.
About Stage 4 CKD
Stage 4 CKD means you have severe loss of kidney function.
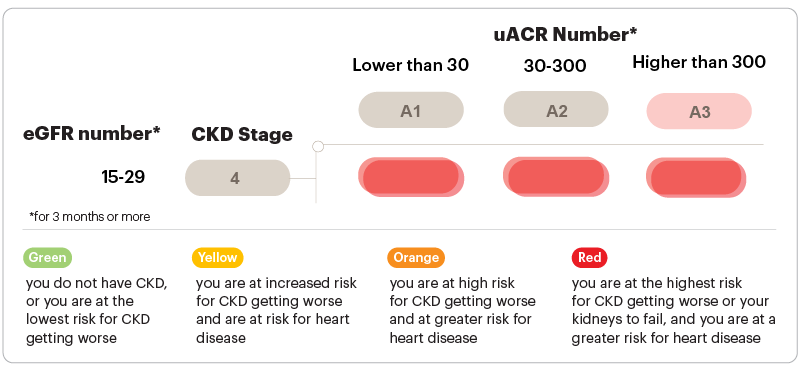
People with stage 4 CKD have an estimated glomerular filtration rate (eGFR) between 15 and 29 for 3 months or more (confirmed with repeat testing to make sure you don’t have acute kidney injury). Another way to think about these numbers is your kidneys are working at 15-29% of what the average two healthy kidneys in a young person can do.
Although urine albumin-creatinine ratio (uACR) results are not needed to confirm CKD at this stage, getting your uACR checked is still important to gain a full picture of your kidney health, as shown in the graphic below.
Health risks with stage 4 CKD
In stage 4 CKD, you are at the highest risk for having kidney failure and you are at very high risk for heart disease (even if your uACR is lower than 30). As your uACR number goes up, your risks of developing heart disease and kidney failure both go up. Getting your uACR level down as low as possible can still help lower your risk, even if you are not able to get your uACR level into the goal range.
CKD complications
Stage 4 CKD is also when complications from kidney disease often appear. These complications include:
- Anemia (low levels of red blood cells)
- Metabolic acidosis (buildup of acid in the blood)
- Mineral and bone disorder (when blood levels of calcium and phosphorus are out of balance leading to bone and/or heart disease)
- Hyperkalemia (high levels of potassium in the blood)
In stage 4 CKD, it is important to have regular check-ups with your healthcare professional to continue to monitor for these complications (usually 4 or more times per year). Each of these complications can be monitored with simple blood tests ordered by your healthcare professional.
People with stage 4 CKD are also at increased risk of developing high blood pressure. So, it is important to have your blood pressure checked regularly.
Signs and symptoms
Symptoms are common in stage 4 CKD and can include:
- Urinating (peeing) more often or less often than usual
- Itchy and/or dry skin
- Feeling tired
- Trouble concentrating
- Numbness or swelling in your arms, legs, ankles, or feet
- Achy muscles or cramping
- Shortness of breath
- Nausea and/or vomiting
- Loss of appetite
- Trouble sleeping
- Breath smells like ammonia (also described as urine-like or “fishy”)
There are many things you can do now to slow down or stop your CKD from getting worse. Sadly, even if you get treatment and are careful about your health, your kidneys may still fail. Still, any steps you take now to improve or maintain your health can still help you in the long term.
Lifestyle recommendations
Now is a great time to make healthier lifestyle choices:
- If you smoke and/or use tobacco products, stop. Smoking can speed up the kidney disease process and increase your risk of getting kidney failure. It also increases your risk for other serious health problems, including high blood pressure, heart disease, cancers, and stroke.
- Exercise regularly. Remember, it’s okay to start slowly – taking short walks is a great way to begin.
- Sleeping well is important, too. Try to get enough sleep so you are well-rested.
- If you are overweight, losing weight through a balanced diet and physical activity can help improve your health in many ways.
- Find ways to reduce and manage stress in your life.
Nutrition
With stage 4 CKD, it is very likely that you will need to change the kinds of foods you eat.
It will be important to limit your sodium (salt) intake to less than 2300 mg per day (about 1 teaspoon of salt from all the food and drinks you consume each day). Your healthcare professional may advise an even lower target depending on your other health conditions. This means a lot more than not using a saltshaker, but also limiting foods with high levels of sodium listed on their nutrition facts label. Some foods that don’t taste salty can have a surprising amount of sodium when you check their nutrition facts label.
Based on the results of your blood tests, your healthcare professional or kidney dietitian may also advise you to change how much potassium, phosphorus, calcium, and/or protein you might be getting through your diet.
Recommendations are highly customized to your body’s specific needs and dietary preferences. So, ask your healthcare professional or kidney dietitian for potential dietary recommendations tailored to you.
Meeting with a dietitian can be especially helpful if you also have other health conditions like diabetes or heart failure where it may be important to limit other types of foods. It can feel overwhelming to keep track of so many changes, and a dietitian can help you identify what works best for you.
Additional information about eating healthy with kidney disease can be found on the Nutrition and Early Kidney Disease page.
Medications
In stage 4 CKD, some of your medications may start to build up in your body. This is because about half of all FDA-approved medications are removed from the blood by your kidneys. Stage 4 CKD is also when it can become unsafe to take some medicines. Ask your healthcare professional or pharmacist if any of your medication doses need to be lowered or if any medicines need to be stopped because of your stage 4 CKD. Some medications may be best avoided or limited in use as well.
Your healthcare professional may also prescribe one or more medicines to help slow down or stop your CKD from getting worse. These medicines include an ACE inhibitor/ARB, an SGLT2 inhibitor and/or an nsMRA.
Your healthcare professional may also prescribe a statin (cholesterol medicine). Guidelines recommend statins for people with stage 4 CKD who also have diabetes, a history of heart disease, or are age 50 or older. Even if you do not have high cholesterol, a statin can help lower your risk of having a heart attack or stroke.
You may also need to take additional medications or supplements to manage any CKD complications you might have (if applicable).
Always bring an updated list of any medications, vitamins, supplements, and herbal medicines you are taking to all your medical appointments and share it with your healthcare professional. Check with your healthcare professional or pharmacist before starting any supplements, herbal medicines, or other over-the-counter products
Other ways to lower your risk
In stage 4 CKD, lowering your risk for CKD progression is very important. This includes taking steps to manage other health conditions you may also have, including high blood pressure (hypertension), diabetes, and high cholesterol.
People with stage 4 CKD should also avoid certain pain medicines known as non-steroid anti-inflammatory drugs (NSAIDs). These can be harmful to your kidneys, especially at higher doses and/or with long-term use. Some examples include:
- ibuprofen (Motrin, Advil)
- indomethacin (Indocin)
- naproxen (Aleve, Naprosyn)
- diclofenac tablets or capsules (Cataflam, Zipsor)
- celecoxib (Celebrex)
- meloxicam (Mobic)
- aspirin (only if more than 325 mg per day)
Many of these medicines are available over the counter and may be sold under a different name or be mixed with other ingredients (like cough & cold medicines). Sometimes it may not be possible to avoid using these products depending on your other health conditions. Always ask your healthcare professional before using any products with these drug names or if the word “NSAID” is printed on the product’s label. In general, acetaminophen, also called Tylenol, is safe for your kidneys at recommended doses - but check with your healthcare professional first to determine the cause of your pain and the best way to treat it.
If your healthcare professional says you have metabolic acidosis, increasing the amount of fruits and vegetables you eat everyday can help lower the level of acid in your blood. This can also help slow down your CKD progression (worsening).
Additional considerations
In stage 4 CKD, it can be helpful to start learning about the different options available for treating stage 5 CKD (kidney failure). Knowing more about your options can help you plan early. Many people who are on dialysis or waiting for a kidney transplant report wishing they had started researching options earlier.
If you are thinking about getting a kidney transplant (even if you are not 100% sure), know that the entire process takes time. So, you may consider taking steps now to start the process. You’ll need to find the right transplant center for you, complete the transplant evaluation, and decide whether to find a living kidney donor or sign up for the kidney transplant waitlist. If you are able to be evaluated and find a living kidney donor soon enough, it may be possible to get the transplant before needing to start dialysis (also known as a preemptive transplant). If you are thinking about signing up for the transplant waitlist and have an eGFR of 20 or less, contact a transplant center to get evaluated so you can begin building your “wait time” on the deceased donor transplant list.
For more information about things to consider, visit the following resources:
Questions to ask
Lowering risk
- Am I at a healthy weight?
- Is my blood pressure within the recommended goal range?
- Do I have diabetes or prediabetes? If so, is my A1C within the recommended goal range?
- Do I have albuminuria?
- How high is my level of risk for developing heart disease or a stroke? What can I do to lower my risk?
Monitoring
- What are my eGFR and uACR numbers?
- When should I have my eGFR and uACR tested again?
- What is my bicarbonate level? If it is below the goal level, what can I do to bring it up?
Medication safety
- Are the medications I am taking safe for me with stage 4 CKD?
- Should the dose of any of my medicines be lowered to prevent side effects or other problems?
Steps to take
- Are there any changes I should make to my diet?
- Are there any ingredients or foods that I should eat less of or avoid?
- Should I take any medication(s) to help lower my risk for CKD getting worse?
- Can you refer me to a kidney dietitian to help me make healthier food choices?
- Can you refer me to a nephrologist (kidney specialist)?
- Is there a kidney disease education program in the area that you can refer me to so I can learn more?
- Do I have any CKD complications like anemia, metabolic acidosis, or mineral and bone disorder? If so, is there anything I should be doing to help manage them?
Planning ahead
- When do you think I will need to start kidney failure treatment, such as dialysis or kidney transplant? Where do I start with this process? What are my options, and can I decide not to have dialysis or a transplant?
- Can you share any information about the closest dialysis and transplant centers to me so I can start to research my options?
Living Well With Kidney Failure
- What kidney failure is and how it affects your body
- Treatment options for kidney failure
- Overcoming challenges that can come with kidney failure
First Steps to Transplant
Free, self-paced online videos about the transplant evaluation and how to get on the waitlist.

Are you coping with kidney disease?
We can help! We can connect you with another kidney patient to talk about kidney disease, dialysis, transplant, or living kidney donation.