Overview
Chronic Kidney Disease (CKD) is silently ushering 37 million of American adults to heart disease, kidney failure and death – and most of them – fully 90%1 -- are unaware of it. As 1 in 3 adults is at risk for the condition, which is associated with high morbidity, mortality, and cost, the argument for action to protect kidney health and intercept this growing public health crisis applies across every stakeholder.
CKDintercept, a major public health initiative of the National Kidney Foundation, offers transformative population health strategies for dramatic risk reduction against both kidney and cardiovascular disease. Working together with primary care providers, laboratories, hospital systems, specialists, public and private insurers, and public health agencies from the federal government to state and local officials, CKDintercept is inculcating evidence-based best practices and successfully driving large scale change in screening, recognition, and management of chronic kidney disease.
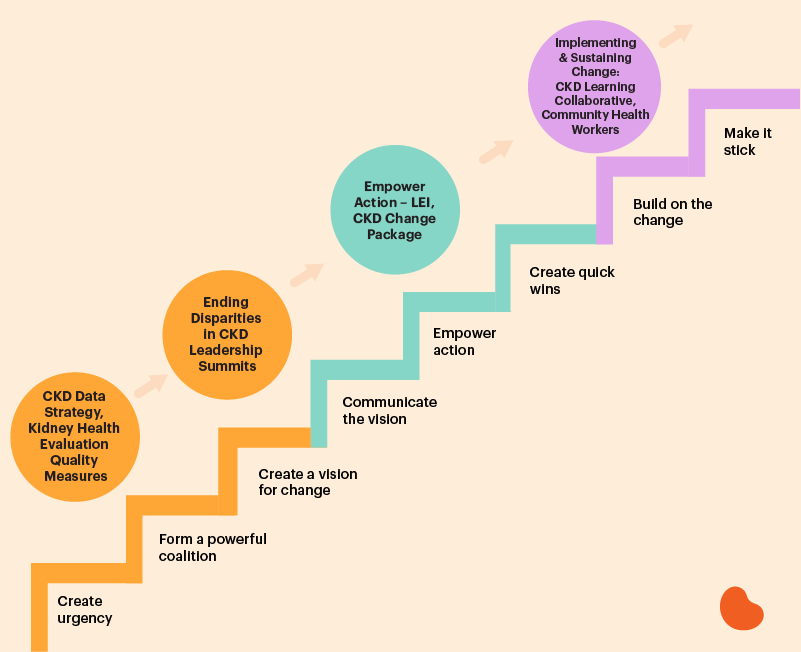
NKF's CKDintercept Population Health "Roadmap"
The Quality & Equity Imperative
Two inexpensive, widely available, and complementary laboratory tests detect CKD. Nevertheless, medical record reviews demonstrate that guideline concordant CKD testing rates among at-risk individuals are abysmal. Hypertension and diabetes are the top two risk factors for CKD, and yet a strong majority of people with these conditions have not had both tests needed to diagnose CKD, including:
- 94% of people with hypertension,
- 61% of people with diabetes,
- 60% of people with BOTH hypertension and diabetes.2
But even when laboratory testing occurs and suggests that a patient has CKD, the information often fails to lead to a diagnosis, management strategy, or referral.3 Up to 90% of patients are unaware of their condition.1
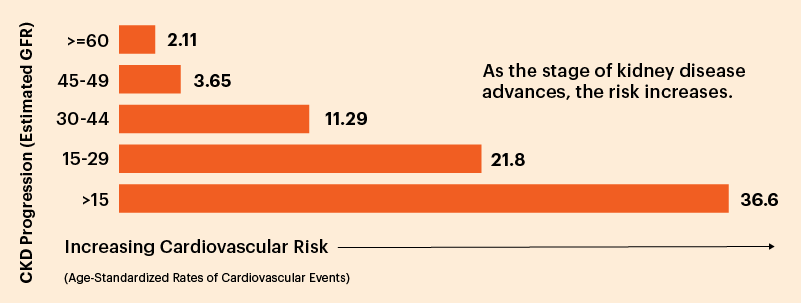
The correlation between kidney and heart disease is well established. Significant science indicates that measures of kidney damage and function are key indicators of cardiovascular disease risk.4. Indeed, the risk of heart disease increases tenfold from early (stage 2) CKD to late (stage 5) CKD.5 It is well established that people with lower kidney function and higher kidney damage are more likely to die of cardiovascular disease than end stage renal disease, making heart disease the leading cause of death for people with kidney disease.6
CKD increases risk for Cardiovascular Disease (heart attacks, strokes, etc.)
Recognition of all risk factors for CKD together with increased screening, diagnosis and disease management are critical to addressing this public health crisis. Beyond hypertension and diabetes, risk factors include overweight/obesity, age (being over 60), and a family history of the condition.
It is difficult to argue that high quality care has occurred if a patient learns they have CKD while in recovery from a heart attack.
To inform and incentivize care providers and to improve testing and diagnosis of CKD, the NKF has developed new HEDIS and MIPS measures for people with diabetes. 2021 reporting year data shows across payer types, an average of only 33-45% of patients were appropriately tested.7
It is important to recognize that CKD occurrence does not discriminate based on broad genetics, race, ethnicity, culture, geography, insurance status, access to care, education, or socio-economic factors. However, disparities in diagnosis, management and referral for specialty care definitively place communities of color at far greater risk of progression to later disease stages.8,9,10
Framing care management to address the structural barriers and social determinants of health that conspire to hasten progression of kidney disease and cardiovascular disease is a quality and equity imperative.
Stopping CKD isn't about "who" the patient is, but about "how" their care is managed. In the absence of equity there can be no quality.
Ending disparities in the care management of all communities is a significant component of the CKDintercept initiative. NKF uses a collective impact model to drive local improvements in CKD population health at the community level, with an emphasis on improving rates of testing and early diagnosis.
The Business Case
The health care cost burden of CKD is substantial and growing. As discussed, CKD is a significant cost multiplier. Patients with CKD commonly often have other comorbidities including diabetes, hypertension and/or other cardiovascular conditions. Within the Medicare Fee-for-Service (FFS) population, 2017 data show that while 14.5 percent of beneficiaries had a diagnosis of CKD, more than half (53.4%) had at least one other comorbid condition (diabetes or cardiovascular disease), 20.2% had two or more, and 5.0% had all three.11
In traditional (FFS) Medicare alone, costs have grown steadily (except in 2020 when COVID-19 impacted access to testing, diagnosis, and care, and increased mortality rates for CKD patients infected by the virus).
| 2016 | 2017 | 2018 | 2019 | |
| Total costs | $114 Billion | $120 Billion | $130.2 Billion | $138.2 Billion |
| ESKD only (including dialysis, kidney transplants) | $35 Billion | $36 Billion | $49.2 Billion | $51.0 Billion |
| % total expenses, CKD, only | 25% | 25.2% | 23.8% | 23% |
| % beneficiaries w/ recognized CKD | 14% | 14.5% | 13.1% | 13.6% |
As sizeable as this cost and illness burden is, however, it almost certainly under-represents the true burden of CKD, since fully one in three American adults is at risk for CKD, but most do not receive appropriate testing to get an early diagnosis or appropriate intervention.
“The burden of CKD on patients and the health care system has been enormous. However, research has shown us that effective interventions and innovative payment models—if designed appropriately—have the potential to generate tremendous savings through improving care for patients with advanced CKD.”
-Lui et al, JASN 2018
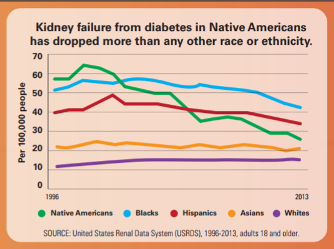
However, population health programs within at-risk communities have demonstrated striking efficacy. For example, the Indian Health Service and the Centers for Disease Control and Prevention (CDC) reported a 54% decrease in the incidence of kidney failure among American Indian and Alaska Native people with diabetes. These remarkable results followed efforts to integrate better care for kidney disease within the context of routine primary care using data-enabled strategies to ensure annual CKD screening and ongoing education for primary care teams.
CKDintercept Program Components
- CKD Data Analysis Strategy: Use existing data to assess and address chronic kidney disease (CKD) in at-risk populations.
- Kidney Health Evaluation Quality Measures: The NKF has developed HEDIS and MIPS measures to improve CKD assessment in primary care.
- Ending Disparities in Chronic Kidney Disease: NKF Leadership Summits: Utilizing the Collective Impact model , these activities convene diverse healthcare and public health stakeholders to develop local strategies to improve CKD population health in their communities.
- Laboratory Engagement Initiative (LEI): U.S. Clinical Laboratories Lead the Way in Advancing Early Diagnosis of Chronic Kidney Disease
- CKD Change Package: The contents of this document represent a list of suggested process improvements that ambulatory care can utilize to improve chronic kidney disease (CKD) screening, recognition and management.
- Chronic Kidney Disease Learning Collaborative: CKD quality improvement initiative to increase routine testing, ensure proper diagnosis, and enhance patient management in primary care settings.
- Community Health Workers: Community Health Workers (CHW) play an important role in the prevention of CKD by educating and helping the communities they serve. The NKF is developing training materials for CHWs to understand CKD.
- Patient Education: Risk tool-driven patient education that tailors the learning experience for each learner to the severity of their CKD and reported complications.
References
- Chronic Kidney Disease in the United States, 2021 (Centers for Disease Control and Prevention,) (2021).
- United States Renal Data System. 2016 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
- Szczech LA, Stewart RC, Su H-L, et al. Primary Care Detection of Chronic Kidney Disease in Adults with Type-2 Diabetes: The ADD-CKD Study (Awareness, Detection and Drug Therapy in Type 2 Diabetes and Chronic Kidney Disease). PLOS ONE. 2014;9(11):e110535. doi:10.1371/journal.pone.0110535
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4119330/
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization [published correction appears in N Engl J Med. 2008;18(4):4]. N Engl J Med. 2004;351(13):1296-1305. doi:10.1056/NEJMoa041031
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.050686
- National Committee on Quality Assurance. Kidney Health Evaluation for Patients with Diabetes (KED). https://www.ncqa.org/hedis/measures/kidney-health-evaluation-for-patients-with-diabetes/
- Scholle SH, Onstad K, Hart A, Hwee T; National Committee for Quality Assurance (NCQA). Chronic kidney disease disparities: educational guide for primary care. Washington, DC: Department of Health and Human Services (DHHS), Centers for Medicare & Medicaid Services (CMS), Office of Minority Health (OMH); February 2020. [Pages 6 & 10] PDF: https://www.cms.gov/files/document/chronic-kidney-diseasedisparities-educational-guide-primary-care.pdf
- United States Renal Data System (USRDS). 2021 USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2021.
- American Society of Nephrology (ASN). Why do minorities have higher rates of kidney failure? (media release). ASN website. 2020, October 23. https://www.asn-online.org/about/press/releases/ASN_PR_20201023_ YanKWFINAL10.24.2020.pdf
- USRDS Annual Data Reports 2016-2021 https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds/prior-data-reports
- Bullock A, Burrows NR, Narva AS, et al. Vital Signs: Decrease in Incidence of Diabetes-Related End-Stage Renal Disease among American Indians/Alaska Natives — United States, 1996–2013. Vol. 66(01). 2017:26-32. Morbidity and Mortality Weekly Report.