National Kidney Foundation and CareFirst partnered for the first time on landmark study
New York, NY – November 12, 2019 - A new study conducted by the National Kidney Foundation and CareFirst BlueCross BlueShield (CareFirst) found that detecting chronic kidney disease (CKD) with two simple tests and treating it based on severity can improve health outcomes for patients with diabetes and hypertension and lower the cost of caring for them.
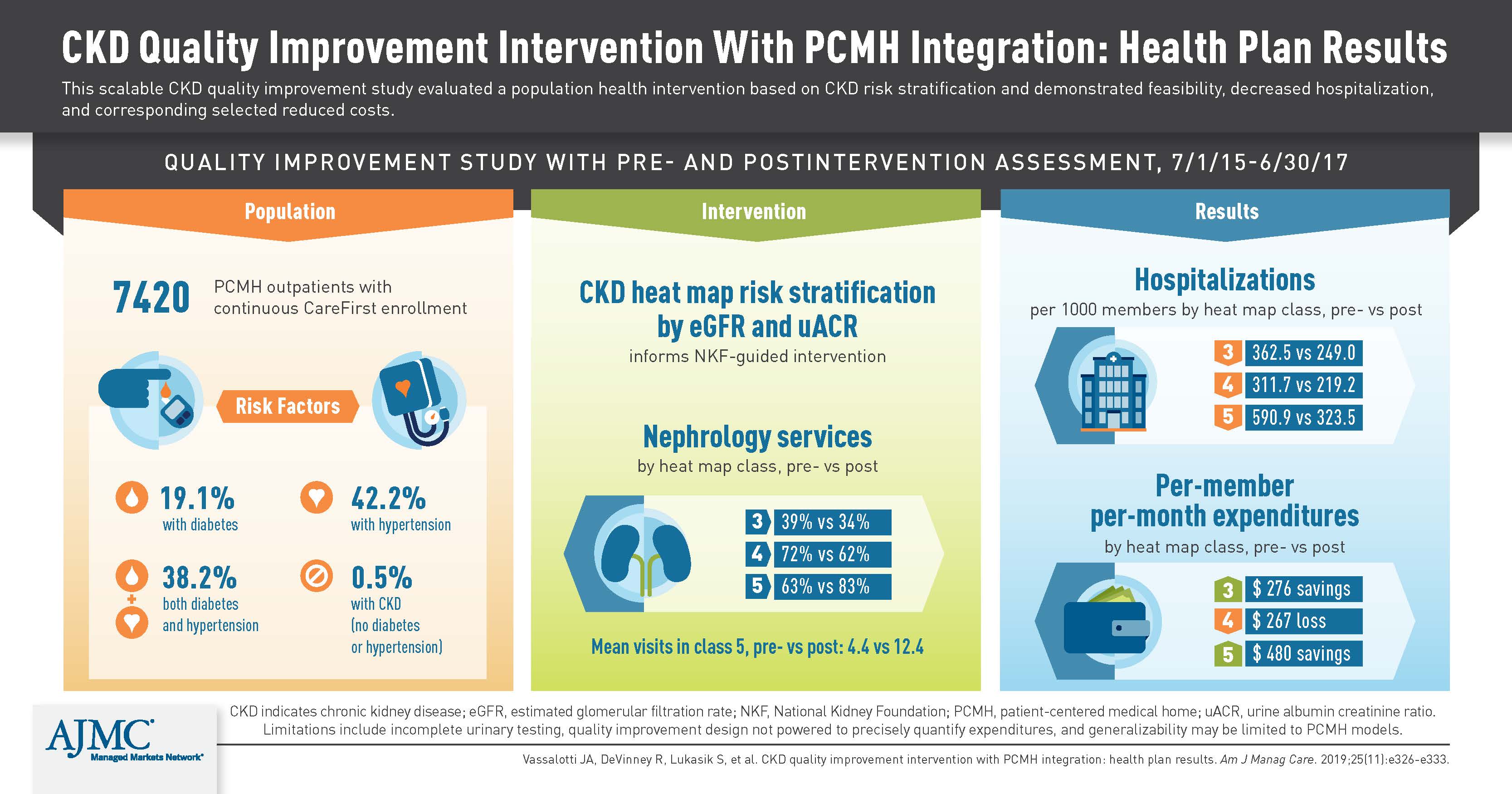
Primary care physicians (PCPs) who used the inexpensive, underutilized urine albumin-creatinine ratio (uACR) test in combination with the more common eGFR blood test, which is also called the estimated Glomerular Filtration Rate, were able to better diagnose the severity of CKD and develop treatments that reduced hospital stays and readmissions, according to the study.
Conducted on more than 7,000 patients in CareFirst’s Patient-Centered Medical Home (PCMH) program from July 2015 to July 2017, the study helped PCPs save thousands of dollars per year per patient on certain healthcare costs, said Dr. Joseph Vassalotti, NKF’s Chief Medical Officer and a co-author of the study, titled CKD Quality Improvement Intervention with PCMH Integration: Health Plan Results.
“This study shows that the combination of both tests for CKD predict adverse outcomes including hospitalizations and 30-day readmissions as well as expenditures,” he said. “A simple, scalable CKD quality improvement intervention stratified by the test results showed short-term improvements in hospitalization and expenditures.”
An estimated 37 million American adults have CKD, but only 10 percent know it. One in three American adults are at risk of developing CKD. Only about 40% of American adults with diabetes receive an annual uACR test for kidney disease as recommended by the American Diabetes Association and the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative. In addition, these are the first real world data, to our knowledge, to show that expenditures increase by albuminuria classification or higher levels of uACR consistently both pre- and post-intervention.
“Chronic kidney disease is under-recognized by the public and, in many cases, under-diagnosed by physicians,” said CareFirst Chief Medical Officer Dr. Daniel Winn, a co-author of the study. “The traditional, standard ways to diagnose CKD are useful, but they’re not a complete, comprehensive screening. The uACR and eGFR tests taken together help categorize kidney disease and give physicians the information they need to develop the most appropriate treatment plans for their patients.”
Among the 7,420 patients treated during the study:
- The mean age per patient was 55.9 years;
- Nearly 52% were women;
- 19.1% had diabetes;
- 42.2% had hypertension; and,
- 38.2% had both conditions.
NKF and CareFirst, an independent licensee of the Blue Cross and Blue Shield Association, worked together to train hundreds of CareFirst employees and community clinicians, including PCPs, nurses, nephrologists, and nutritionists. Modest changes in testing and therapies -- including medical nutrition therapy and informed selection of nephrology practitioners by increasing nephrology services for advanced CKD -- contributed to the positive results.
“Health insurance plans and health systems should consider following CareFirst’s lead to design a similar intervention and train their teams in this effort because CKD quality improvement can significantly reduce costs and more importantly, improve patient outcomes,” Dr. Vassalotti said.
The authors of the study were Dr. Vassalotti of NKF and Icahn School of Medicine at Mount Sinai, New York; Rachel De Vinney, MPH, CHES, of CareFirst; Stacey Lukasik, BA, of CareFirst; Sandra McNaney, BS, CareFirst; Elizabeth Montgomery, BS, NKF; Cindy Voss, MA, CareFirst; and Daniel Winn, MD, CareFirst.
The study will be published today in The American Journal of Managed Care, a peer-reviewed journal with a large readership among the healthcare payer community. The article will be available by going to: https://www.ajmc.com/journals/issue/2019/2019-vol25-n11/ckd-quality-improvement-intervention-with-pcmh-integration-health-plan-results.
About CareFirst BlueCross BlueShield
In its 82nd year of service, CareFirst, an independent licensee of the Blue Cross and Blue Shield Association, is a not-for-profit health care company which, through its affiliates and subsidiaries, offers a comprehensive portfolio of health insurance products and administrative services to 3.2 million individuals and groups in Maryland, the District of Columbia and Northern Virginia. In 2018, CareFirst invested $38 million to improve overall health, and increase the accessibility, affordability, safety and quality of health care throughout its market areas. To learn more about CareFirst BlueCross BlueShield, visit our website at www.carefirst.com or follow us on Facebook, Twitter, LinkedIn, or Instagram.
About The American Journal of Managed Care®
The American Journal of Managed Care® (AJMC®) is a multimedia peer-reviewed, MEDLINE-indexed journal that keeps industry leaders on the forefront of health policy by sharing digital research relevant to industry decision-makers. Other brands in the AJMC® family include The American Journal of Accountable Care®, Evidence-Based Oncology™ and Evidence-Based Diabetes Management™. These comprehensive multimedia brands bring together stakeholder views from payers, providers, policymakers and other industry leaders in managed care. AJMC® is a brand of MJH Life Sciences™, the largest privately held, independent, full-service medical media company in the U.S. dedicated to delivering trusted health care news across multiple channels.
NKF Professional Membership
Healthcare professionals can join NKF to receive access to tools and resources for both patients and professionals, discounts on professional education, and access to a network of thousands of individuals who treat patients with kidney disease.
Kidney Disease Facts
In the United States, 37 million adults are estimated to have chronic kidney disease (CKD) – and most aren’t aware of it. 1 in 3 American adults is at risk for CKD. Risk factors for kidney disease include diabetes, high blood pressure, heart disease, obesity, a family history of kidney failure, and being age 60 or older. People of African-American, Hispanic, Native American, Asian or Pacific Islander descent are at increased risk for developing the disease. African-Americans are about 3 times more likely than Whites to develop end-stage kidney disease (ESKD or kidney failure). Compared to non-Hispanics, Hispanics are almost 1.3 times more likely to receive a diagnosis of kidney failure.
The National Kidney Foundation (NKF) is the largest, most comprehensive, and longstanding patient-centric organization dedicated to the awareness, prevention, and treatment of kidney disease in the U.S. For more information about NKF, visit www.kidney.org.