Key Points: Living With Stage 4 Kidney Disease
Contents
If you have stage 4 kidney disease, it is important for you to:
- Learn what you can do to keep kidney disease from getting worse - and do it!
- Do your part to manage the complications of kidney disease
- Heart and blood vessel problems
- Anemia (low red blood cell count)
- Bone problems
- High blood pressure
- Poor nutritional health (i.e. happens when you are not getting enough important nutrients and energy for your body to function and stay healthy)
- Learn more about kidney failure and the different treatment options for it.
What is Stage 4 Kidney Disease?
Chronic kidney disease (CKD) happens if your kidneys have been damaged. Kidneys can become damaged from a physical injury or a disease like diabetes or high blood pressure. Once your kidneys are damaged, they are not able to filter blood or do their other jobs well enough to keep you healthy. Some of the important jobs kidneys do:
- Filter blood
- Balance your body's fluids
- Regulate hormones
- Help keep blood pressure under control
- Keep bones healthy
- Help make red blood cells
There are five stages of chronic kidney disease. The mildest are stages 1 and 2. In these early stages of kidney disease, the kidneys are damaged and not working at full strength. At stage 3, about half of kidney function has been lost. This can cause other problems, like high blood pressure or bone problems. Treatment of these problems is very important, and it can even help slow down the loss of kidney function. At stage 4, severe kidney damage has happened. At this stage, it is very important to slow the loss of kidney function by following your treatment plan, and managing other problems like high blood pressure or heart disease. Stage 5 is kidney failure. If kidney failure happens, you will need a kidney transplant or dialysis to live.
Learn About Kidney Failure
Even if you get treatment in stage 4 and are careful about your health, your kidneys may still fail. Kidney failure happens when:
- 85-90% of kidney function is gone
- GFR falls below 15
- Kidneys don't work well enough to keep you alive
There is no cure for kidney failure, but with treatment it is possible to live a long, fulfilling life. Having kidney failure is not a death sentence. People with kidney failure live active lives and continue to do the things they love.
Treatments for Kidney Failure
The two treatments for kidney failure are kidney transplantation and dialysis. Two different types of dialysis can be done - hemodialysis and peritoneal dialysis.
- Kidney Transplantation. This is an operation that places a healthy kidney into your body. The kidney can come from someone who has died or from a living donor. A new kidney will usually function immediately. You will need special medicines to prevent your body from rejecting the new kidney. If rejection happens, dialysis is needed and you can consider a second transplant. A kidney transplant is a treatment, not a cure. Kidney transplant recipients still have chronic kidney disease, and you may still need some of the other medicines you took before the transplant.
- Hemodialysis (HD). Hemodialysis is a treatment that removes wastes and extra fluid from your blood. It can be done at home ("home hemodialysis") or in a dialysis center. During hemodialysis, your blood is pumped through soft tubes to a dialysis machine where it goes through a special filter called a dialyzer (also called an artificial kidney). As your blood is filtered, it is returned to your blood stream. Only a small amount of blood is out of your body at any time. In-center treatment time is 3-5 hours, 3 times a week. People who do home hemodialysis have more flexibility about how often it can be done. If done daily, treatment time would be 1½ to 2 hours. You will need an access into the bloodstream for placing needles needed for hemodialysis. Types of access include:
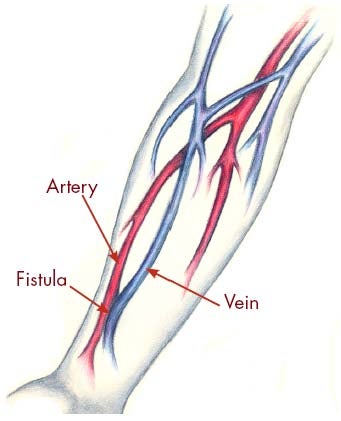 Fistula. A fistula is the recommended choice for an access. You will need a minor operation to create a fistula. It is made by joining an artery to a nearby vein under your skin to make a bigger blood vessel. This type of access is preferred because it has fewer problems and lasts longer. However, some people may not be able to have a fistula because of their physical condition. Sometimes, it may be possible to switch to a fistula from another type of access. If you do not have a fistula, ask your dialysis care team if a switch would be possible.
Fistula. A fistula is the recommended choice for an access. You will need a minor operation to create a fistula. It is made by joining an artery to a nearby vein under your skin to make a bigger blood vessel. This type of access is preferred because it has fewer problems and lasts longer. However, some people may not be able to have a fistula because of their physical condition. Sometimes, it may be possible to switch to a fistula from another type of access. If you do not have a fistula, ask your dialysis care team if a switch would be possible.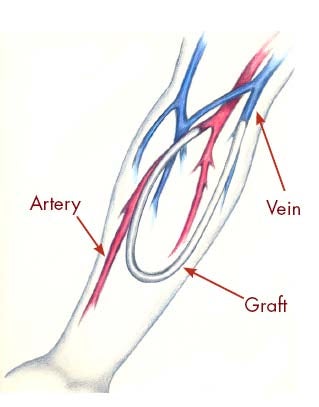 Graft. If your blood vessels are not suitable for a fistula, a graft may be used. This involves joining an artery and a nearby vein with a small, soft tube made of synthetic material. The graft is entirely beneath your skin. You will need a minor operation to create a graft.
Graft. If your blood vessels are not suitable for a fistula, a graft may be used. This involves joining an artery and a nearby vein with a small, soft tube made of synthetic material. The graft is entirely beneath your skin. You will need a minor operation to create a graft.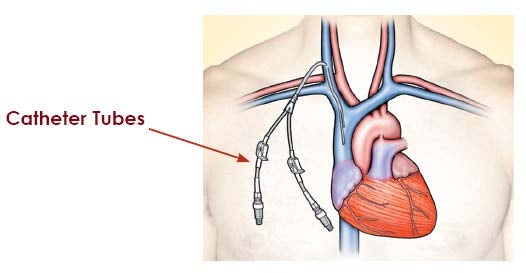 Catheter. The third type of access, called a catheter, is inserted into a large vein in your neck or chest. The ends of the tubes sit on your skin outside your body. This type of access is generally used when you need dialysis for a short period of time. Catheters are used as a permanent access when a fistula or a graft cannot be placed.
Catheter. The third type of access, called a catheter, is inserted into a large vein in your neck or chest. The ends of the tubes sit on your skin outside your body. This type of access is generally used when you need dialysis for a short period of time. Catheters are used as a permanent access when a fistula or a graft cannot be placed.
- Peritoneal Dialysis (PD). Peritoneal dialysis is a home-based treatment that can be done anywhere (at home, work, or when sleeping). It must be done daily. You will need a minor operation to place a catheter in your abdomen (belly). With peritoneal dialysis, the blood is cleaned inside your body, not outside. The lining of your abdomen (the peritoneum) acts as a natural filter. During treatment a cleansing solution, called dialysate, flows into your abdomen (your belly) through a soft tube called a PD catheter. Wastes and extra fluid pass from your blood into the cleansing solution. After several hours, you drain the used solution from your abdomen and refill with fresh cleansing solution to begin the process again. Removing the used solution and adding fresh solutions takes about a half hour and is called an "exchange."
To learn more about each type of treatment, see "Choosing a Treatment for Kidney Failure" in the A-to-Z Guide.
Can You Change Treatments for Kidney Failure?
If you start on one type of treatment for kidney failure but feel you would like to try something else, you can speak to your healthcare professional about changing. For most people, it is often possible to change treatments. For example, if you choose hemodialysis, it doesn't mean you can't switch to peritoneal dialysis at a later date. Even if you choose to have a kidney transplant, you may need a period of dialysis until you can be transplanted with a new kidney. It is not uncommon for people who have had kidney failure for many years to have had more than one type of treatment in that time.
Help Keep Your Kidney Disease from Getting Worse
Good self-management will help you to live a long, fulfilling life and continue to do the things you love. It can also help to slow or even stop kidney disease from getting worse - and it may even stop or delay kidney failure. Good self-management starts with:
- Controlling other health problems you may have
- Treating complications of kidney disease
- Managing or preventing heart disease
Control Other Health Problems
You may have other disorders, such as diabetes and high blood pressure, which can damage your kidneys. One of the goals of your treatment is to make sure these are well-controlled. Ask your healthcare professional what you can do to keep these conditions under control - and do it! Some of the things your healthcare professional may ask you to do:
- Take medications called angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) as part of your therapy. Studies have shown that these medications help to protect your kidney function. You may also need other blood pressure medications to control your blood pressure.
- Lose weight if you are overweight
- Cut down on salt in your diet to control blood pressure
- If you have diabetes, monitor your blood sugar, follow your diet and take your medications as prescribed
Do What You Can to Manage the Complications of Kidney Disease
Kidney disease can cause other health problems throughout your body including:
- Heart and blood vessel problems
- Anemia (low red blood cell count)
- Mineral and bone problems
- High blood pressure
- Poor nutritional health
If you have stage 4 kidney disease, you are probably experiencing some of these problems already. Your healthcare professional will work with you to develop a treatment plan to help manage these problems and keep them from getting worse. Treatment may include diet, exercise, and medications. It is very important that you follow your treatment plan because it can greatly improve your quality of life and how long you live. It can also help to slow or even stop kidney disease from getting worse - and it may even stop or delay kidney failure.
Manage or Prevent Heart Disease
People with stage 4 kidney disease have a high risk of having heart disease. In fact, most people with kidney disease do not die of kidney failure - they die of heart disease. Why? Because, in addition to kidney disease, they usually have one or more of the following health risks:
- High blood pressure causes arteries to thicken and narrow, making it easier to form clots, which can lead to a heart attack or stroke. It also causes thickening and enlargement of the heart. Your doctor may prescribe medicines to help control your blood pressure. You may also need to reduce salt in your diet.
- Diabetes, especially uncontrolled diabetes, leads to more fatty deposits in arteries. These can form a clot, leading to a heart attack or stroke. If you have diabetes, you must be careful to control your blood sugar, follow your diet, and take your medications as prescribed.
- Anemia reduces the flow of oxygen throughout your body, which forces your heart to work harder. As a result, your heart begins to thicken and enlarge, which can lead to heart failure or death. To treat anemia, you may need to take iron supplements and a medicine called ESA (erythropoiesis-stimulating agents). These will help your body make red blood cells, which helps increase the flow of oxygen.
- Abnormal cholesterol causes fatty deposits to form in your arteries, making it easier to form clots which can lead to a heart attack or stroke. If your cholesterol is too high, your doctor may recommend changes in your diet, regular exercise and, possibly, special medications, to help lower cholesterol.
- Bone and mineral disease causes your arteries to stiffen and narrow from absorbing extra calcium and phosphorus that's being shed from your bones. This reduces blood flow to your heart, which can lead to a heart attack and death. To help control bone and mineral disease, you may need to limit the amount of high-phosphorus foods in your diet, take a type of medication called a phosphate binder with your meals, and take a form of vitamin D.
- Smoking causes inflammation of the blood vessels, which causes even more buildup of fatty deposits in your arteries. Smoking increases the risk of clots, which can lead to a heart attack or stroke. If you smoke, you should smoke less or consider quitting.
You can help slow - or possibly prevent - heart problems by following your treatment plan. Ask your healthcare professional what you need to do to keep your heart healthy.
Tools to Help
Use these self-management tools to help you track your progress and improve your quality of life.
- Track Your GFR and Albuminuria Numbers
- Communicating With Your Healthcare Team
- Know Your Numbers
- Activity Schedule
- Getting Ready for a "New Normal." A Helpful Guide for Starting Dialysis
To learn more
You can learn more about managing stage 4 kidney disease in the A-to-Z guide:

- About Chronic Kidney Disease: A Guide for Patients and Their Families
- GFR
- Choosing a Treatment for Kidney Failure
- Kidney Transplant
- Hemodialysis access: What You Need to Know
- Anemia and Chronic Kidney Disease
- Diabetes and Kidney Disease
- High Blood Pressure and Chronic Kidney Disease
- Peritoneal Dialysis: What You Need to Know
- Diet and Nutrition
- Keep Your Heart Healthy