Evaluation and management of nephropathic cystinosis, including diagnosis, treatment with cysteamine, and lifelong care strategies.
Pathophysiology
Nephropathic cystinosis is an autosomal recessive metabolic disorder. It is a rare disease with a lifelong impact on the patient. The yearly incidence of nephropathic cystinosis is ~1:150,000 to 200,000 live births and its prevalence is ~1.6 per million population.1 However the incidence has been reported to be higher in specific populations globally.2, 3
Cystine is derived from the normal enzymatic degradation of proteins within the cell's lysosomes. Cystine is transported through the lysosomal membrane to the cytosol by cystinosin, a specific lysosomal membrane protein transporter.3,4
Cystinosis is characterized by an accumulation of the amino acid cystine throughout the body, as a result of its impaired transport out of the lysosomes within cells.4 Nephropathic cystinosis is linked with >100 known mutations in the gene CTNS encoding for cystinosin and results in the accumulation of intralysosomal cystine throughout many organs and tissues (Figure 1).1,4
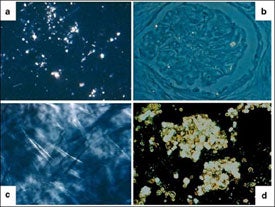
(a) Liver; (b) kidney; (c) cornea; (d) bone marrow
The most frequent known mutation linked with cystinosis among Northern Europeans is a 57-kb deletion that involves the first 10 exons of CTNS, and two other genes - CARKL and TRPV1.6,7,8 The gene CARKL (carbohydrate kinase-like) encodes for the enzyme sedoheptulokinase, and TRPV1 (transient receptor potential cation channel subfamily V member 1) encodes for the transient receptor potential vanilloid.
Clinical Presentation
Cystinosis has three forms of clinical presentation, based on the age at first clinical symptoms: classic infantile/early-onset nephropathic; intermediate/late-onset nephropathic; and adult/ocular non-nephropathic.
Infantile nephropathic cystinosis is the most common form of the disease, accounting for ~95 % of cases. It commonly presents in early infancy with Fanconi syndrome, which consists of multiple defects in renal proximal tubular reabsorption. If left untreated, Fanconi syndrome leads to kidney failure (end-stage renal disease, or ESRD) in the later childhood years.1,9, 10
Children at birth with nephropathic cystinosis are generally asymptomatic and normal in weight and length. The first noticeable clinical signs of infantile cystinosis generally appear between 6 and 12 months of age. Symptoms can include poor growth, feeding intolerance, and episodes of volume depletion (dehydration). These symptoms are due in part to the renal Fanconi syndrome, which is characterized by excessive urinary loss of sodium, potassium, phosphate, calcium, magnesium, and water, along with diminished activation of the kidney produced vitamin D metabolite, calcitriol. These metabolic abnormalities can lead to hypokalemia, hyponatremia, metabolic acidosis, poor weight gain, poor linear growth, rickets in the bones, and/or generalized muscle weakness. Other organs and tissues can also be affected by cystinosis, resulting in retinal, endocrine, and neuromuscular complications as the patient ages. Youth with cystinosis might also have neurocognitive problems, including poor visual-motor integration, sustained attention, visual memory and executive function.
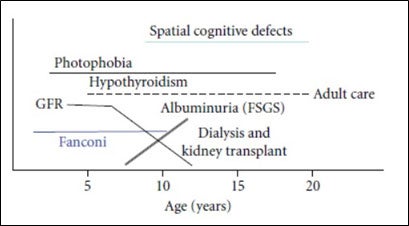
Typically, in the infantile form of nephropathic cystinosis, kidney filtering function declines slowly until the age of 5 years, but loss of function may accelerate thereafter in an untreated patient, leading to kidney failure at about 10-12 years of age (Figure 2).11,12 Prior to the use of cystine-depleting therapy and kidney transplantation, the life span of a child with nephropathic cystinosis was about 10 years. However, with modern and optimal care, patients currently survive into their mid-forties or fifties with a satisfactory quality of life and long-term outcomes are improving.1
Approximately 5% of cystinosis cases are the juvenile (late-onset) nephropathic form. These patients do not have noticeable clinical symptoms until late childhood or adolescence. Clinical manifestations can include mild or absent Fanconi syndrome and asymptomatic proteinuria. They can have nephrotic syndrome, which can be confused with other causes.14 Generally, these patients have a slower progression to kidney failure.
The adult, non-nephropathic ocular form of cystinosis typically only affects the eyes. It is characterized by photophobia due to corneal cystine accumulation, and rarely presents before adulthood.2
Diagnosis
Detection of elevated cystine levels in white blood cells (WBCs) is considered the main diagnostic test for cystinosis. It can also be applied to assess the effectiveness of cystine-depleting therapy. Multiple methods of cystine measurement in WBCs have been developed over time, including cystine-binding protein assays, high-performance liquid chromatography (HPLC), or liquid chromatography-tandem mass spectrometry (LC-MS/MS).1,15,16,17 Tandem mass spectrometry is considered the current method of choice.1, 10
Newly diagnosed patients who have nephropathic cystinosis will almost always have WBC cystine levels in the range of 3 to 20 nmol half-cystine/mg protein.1, 10 It has been suggested that these elevated leukocyte cysteine levels at any age provides a definitive diagnosis. Control individuals and heterozygous carriers have levels ranging from <0.2 to <1.0 nmol half-cystine/mg protein, respectively.1, 10
Molecular testing of the CTNS gene is considered important in genetic counseling and is generally recommended to confirm an initial diagnosis.1 It is not tested for with normal newborn screening. However, CTNS gene testing can be considered in a newborn or fetus with a strong positive family history. CTNS gene testing can reveal ~95% of disease causing mutations.10
Detection of corneal cystine crystals by slit lamp examination is another possible option for confirming diagnosis. However, cystine corneal crystals do not appear with this method until the second year of life. This examination should be performed by an ophthalmologist familiar with the disease to identify and grade the crystal load in the cornea properly.10
Urinalysis in patients with nephropathic cystinosis can show a low specific gravity, overt glucosuria (with normal serum glucose), and mild-to-moderate albuminuria.2 Serum creatinine is usually normal in young children, unless they are dehydrated. Since many children with cystinosis have muscle wasting with poor growth, serum creatinine alone (which is a product of muscle breakdown) may be a poor marker of kidney function.
Cystinosis should be considered in the differential diagnosis of every young patient presenting with kidney failure of unknown origin, particularly if there is a history of polyuria and poor growth.10
Management
In general, management of nephropathic cystinosis involves administration of oral cysteamine therapy and other treatments to care for the Fanconi Syndrome, including fluid and electrolyte management. Any treatment plan should undergo regular evaluation, and be revised to improve care and address emerging issues through the life of the patient as their needs change over time.1, 10,18
Infants diagnosed with nephropathic cystinosis often require more frequent nephrologist visits during infancy and childhood than during adolescence. Monitoring of WBC cystine levels, and other blood-based parameters, every 3-4 months are usually necessary. Other important components of nephropathic cystinosis management in infants and children include appropriate nutritional adjustments as well as fluid and electrolyte management (depending on the presence and severity of Fanconi syndrome).
As a child with nephropathic cystinosis enters adolescence, other special issues and challenges begin to emerge, including adherence to prescribed therapies, increasing likelihood of the development of some extra-renal complications (e.g., hypothyroidism, insulin-requiring diabetes mellitus, type I, neuromuscular complications), progression to kidney failure with the need for renal replacement therapy, and the transition to adult age and adult-provider care.19, 20
As cystinosis patients live further into adulthood, more long-term complications have been observed, as they did not have enough time to evolve in the pediatric age group during the absence of these therapies. Furthermore, the potential also remains for the development of yet undescribed manifestations for patients who have been treated early and appropriately.1, 10
A multispecialty team is recommended for patients with cystinosis, including where applicable, specialists from nephrology/transplant nephrology, neurology, ophthalmology, pulmonology, endocrinology, social workers, psychology, otorhinolaryngology specialized in swallowing dysfunction, orthophonists, and physiotherapists.
Cystine Depleting Therapy
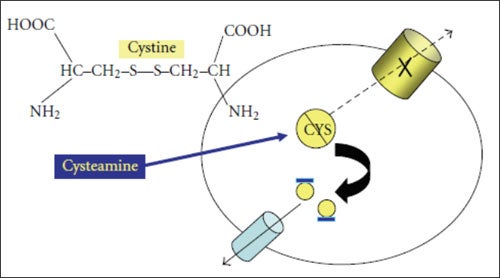
The mainstay of therapy for nephropathic cystinosis is cystine reduction therapy with cysteamine bitartrate compounds. Such therapy reduces lysosomal cystine through the formation of cystine into a mixed disulfide cysteamine-cystine complex that exits the lysosome via an intact PQLC2-transporter (Figure 3).10
The original cysteamine bitartate preparation is now termed immediate-release. With this preparation, the dosage was usually 60 - 90 mg/kg /day or 1.35–1.90 g/m2 body surface area/day, administered every six hours. This formulation had been available in the US and much of the European continent since the 1990s.
In 2013, the FDA approved an every twelve hour, delayed-release formulation of cysteamine bitartrate for the management of nephropathic cystinosis in adults and pediatric patients. In 2015, FDA approval was expanded for children from ≥6 years of age to ≥2 years of age. It reduces the dosing burden from every six hours to every 12 hours daily.18 A prospective, controlled clinical trial demonstrated continued pharmacodynamic efficacy after 24 months of treatment.21
Topical treatment with cysteamine hydrochloride eye drops are administered to treat corneal cystine crystals.18 A commercial 0.44% cysteamine ophthalmic solution was approved by the FDA in 2012 treatment of corneal cystine crystals in cystinosis patients.
Renal Replacement Therapy
Renal Fanconi syndrome can persist after initiation of dialysis or after kidney transplantation in the native kidneys, but only rarely necessitates native nephrectomies, because excessive fluid and electrolyte losses are generally reduced with renal replacement therapy.22 The presence of polyuria and sodium wasting limits the need for ultrafiltration in cystinosis patients on hemodialysis or peritoneal dialysis in those patients with residual kidney function.1,23
Kidney transplantation is the preferred treatment for kidney failure in nephropathic cystinosis. Both living donor and deceased donor kidneys are effective. Overall, kidney transplantation is associated with better outcomes in nephropathic cystinosis than in patients undergoing transplantation for other indications, but continued diligence is required nevertheless.20,22,24
Kidney transplantation does not correct the metabolic defect in other tissues, and cystine continues to accumulate and to cause organ damage. Therefore, treatment with cysteamine continues for life after transplantation. The post-transplant goal of cysteamine therapy is to delay or reverse extrarenal organ damage.20,22
It is crucial for healthcare providers to understand that a patient's cystinosis is not cured after transplantation and multi-disciplinary care is critical to promote long-term health.22 Adherence to prescribed treatments for cystinosis, related conditions, and/or a kidney transplant can be an ongoing challenge for these patients who must manage a complex treatment regimen throughout life.
References
- Langman C, Barshop B, Deschênes G, et al. Controversies and research agenda in nephropathic cystinosis: conclusions from a "Kidney Disease: Improving Global Outcomes" (KDIGO) Controversies Conference. Kidney Int. 2016:89:1192-1203.
- Niaudet P. Cystinosis. Matoo T (Ed). UpToDate, Waltham, MA. Accessed July 6, 2017.
- Gahl W, Thoene J, Schneider J. Cystinosis. N Engl J Med. 2002;347:111-211.
- Gahl W, Thoene J, Schneider J. Chapter 199. Cystinosis: a disorder of lysosomal membrane transport. In: Scriver CR, Beaudet AL, Sly WS, Valle D, Childs B, Kinzler KW, Vogelstein B, eds. The Metabolic and Molecular Basis of Inherited Disease, Eighth Edition. McGraw-Hill Companies; 2001:5085-5108.
- Nesterova G, Gahl W. Nephropathic cystinosis: late complications of a multisystemic disease. Pediatr Nephrol. 2008;23:863-878.
- Taranta A, Wilmer M, van den Heuvel L, et al. Analysis of CTNS gene transcripts in nephropathic cystinosis. Pediatr Nephrol. 2010;25:1263-1267.
- Topaloglu R, Vilboux T, Coskun T, et al. Genetic basis of cystinosis in Turkish patients: a single-center experience. Pediatr Nephrol. 2012;27:115-121.
- Wamelink M, Struys E, Jansen E. Sedoheptulokinase deficiency due to a 57-kb deletion in cystinosis patients causes urinary accumulation of sedoheptulose: elucidation of the CARKL gene. Hum Mutat. 2008;29:532-536.
- Ivanova E, De Leo MG, De Matteis MA, Levtchenko E. Cystinosis: clinical presentation, pathogenesis and treatment. Pediatr Endocrinol Rev. 2014;12(Suppl 1):176-184.
- Elmonem M, Veys K, Soliman N, van Dyck M, van den Heuvel L, Levtchenko E. Cystinosis: a review. Orphanet J Rare Dis. 2016;11:47.
- Greco M. Brugnara M, Zaffanello M, et al. Long-term outcome of nephropathic cystinosis: a 20-year single-center experience. Pediatr Nephrol. 2010;25:259-2467.
- Lucky A, Howley P, Megyesi K, et al. Endocrine studies in cystinosis: compensated primary hypothyroidism. J Pediatr. 1977;91:201-210.
- Goodyer P. The history of cystinosis: lessons for clinical management. Int J Nephrol. 2011;2011:929456.
- Servais A, Morinière V, Grünfeld J, et al. Late-onset nephropathic cystinosis: clinical presentation, outcome, and genotyping. Clin J Am Soc Nephrol. 2008;3:27-35.
- Oshima R, Willis R, Furlong C, Schneider J. Binding assays for amino acids. The utilization of a cystine binding protein from Escherichia coli for the determination of acid-soluble cystine in small physiological samples. J Biol Chem. 1974;249:6033-6039.
- de Graaf-Hess A, Trijbels F, Blom H. New method for determining cystine in leukocytes and fibroblasts. Clin Chem. 1999;45:2224–2228.
- Chabli A, Aupetit J, Raehm M, Ricquier D, Chadefaux-Vekemans B. Measurement of cystine in granulocytes using liquid chromatographytandem mass spectrometry. Clin Biochem. 2007;40:692-698.
- Emma F, Nesterova G, Langman C, et al. Nephropathic cystinosis: an international consensus document. Nephrol Dial Transplant. 2014;29(suppl 4):iv87–iv94.
- Brodin-Sartorius A, Tete M, Niaudet P, et al. Cysteamine therapy delays the progression of nephropathic cystinosis in late adolescents and adults. Kidney Int. 2012;81:179-189.
- Van Stralen K, Emma F, Jager K, et al. Improvement in the renal prognosis in nephropathic cystinosis. Clin J Am Soc Nephrol. 2011;6:2485-2491.
- Langman C, Rioux P, Greenbaum L, et al. Extended treatment of patients with cystinosis and CKD with RP103 demonstrates efficacy and safety. Pediatr Nephrol. 2013;28:1363.
- Wilmer M, Schoeber J, van den Heuvel L, Levtchenko E. Cystinosis: practical tools for diagnosis and treatment. Pediatr Nephrol. 2011; 26:205-215.
- Langlois V, Geary D, Murray L, et al. Polyuria and proteinuria in cystinosis have no impact on renal transplantation: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol. 2000;15:7-10.
- Ehrich JH, Bordehl J, Byrd D, et al. Renal transplantation in 22 children with nephropathic cystinosis. Pediatr Nephrol. 1991;5:708-714.








