Table of Contents
- Identify evidence-based implementation strategies based on published literature and organizational expertise.
- Ensure care team members executing the CKD intervention helped identify implementation strategies aligned with practice or clinic needs and requirements.
- Consider implementation of an electronic health record-based CKD registry.
- Develop the recommended CKD care plan for your institution.
- Consider developing CKD clinical decision support.
- Review / update diabetes and hypertension order sets to include agreed upon CKD parameters including assessment with the Kidney Profile, medication management, referrals.
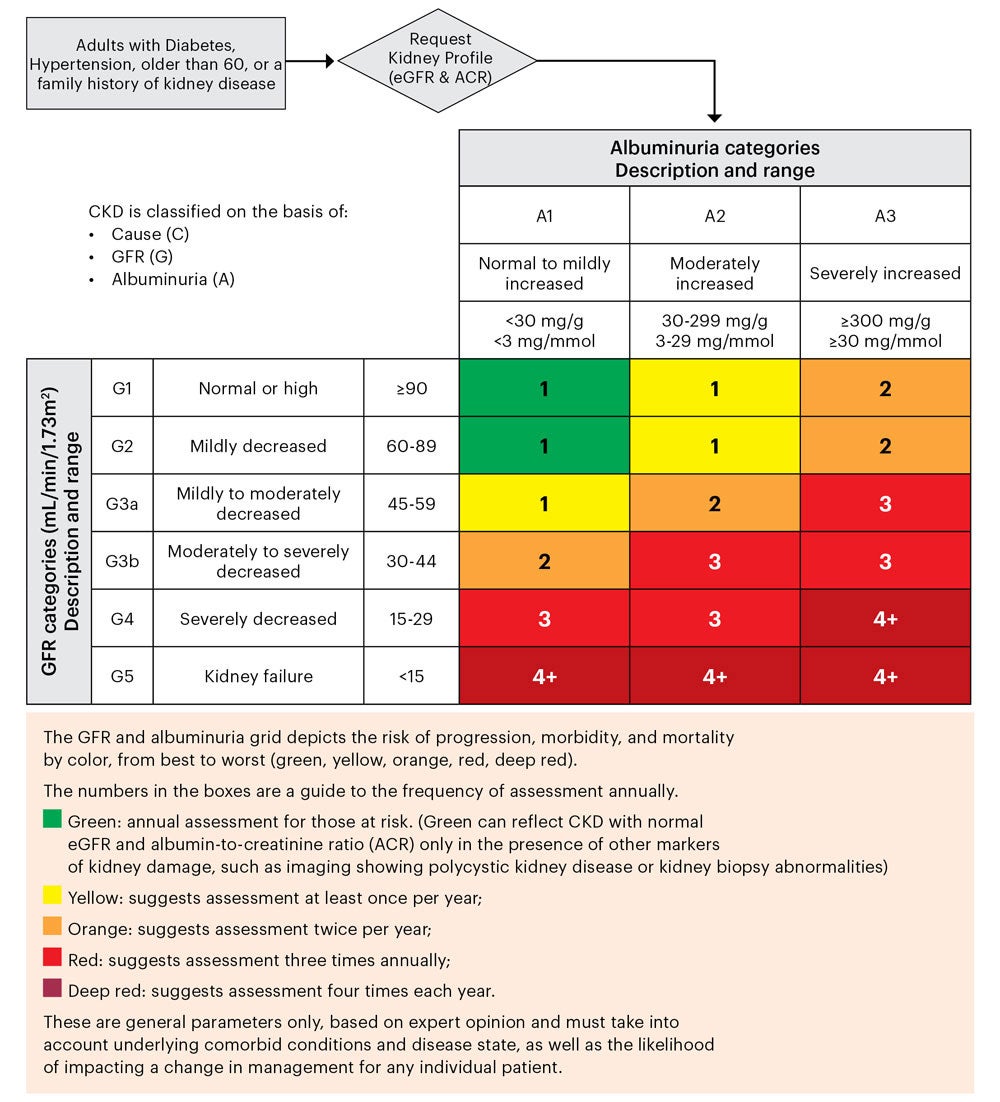
- Consider embedding the CKD heat map in EMR tools to facilitate CKD staging/risk stratification.
- Where appropriate create dot phrases to facilitate entry of CKD information.
- Consider use of the Kidney Health Evaluation for Patients with Diabetes MIPS measure.
- Include social determinants of health assessment in the CKD intervention.
- Consider including resources to address identified social determinants of health needs in the intervention tools.
- Within the context of available resources, consider novel community-level approaches for identified needs related to social determinants of health.
- Outline a seamless communication strategy among patient care team members.
- Make CKD patient education a convenient experience.
- Include referral information for local support groups or peer-mentoring programs.
- Utilize multiple channels of outreach to engage patients around CKD awareness and screening.
- Consider creating a tool kit to address the specific care gap(s) targeted.
- References
Consideration of local practice needs including workflows, patient panels, and available resources is an integral part of planning and development. Following are Resources and Tools that can support these processes.
Identify evidence-based implementation strategies based on published literature and organizational expertise.
Tools:
- American Academy of Family Physicians (AAFP), Basics of Quality Improvement, a summary of quality improvement (QI) basics including benefits and proven QI models and tools.
- American College of Physicians (ACP), Quality Improvement in Healthcare: ACP Resources and Programs, a succinct overview of QI resources that includes QI curriculum, training, coaching, and resources to improve patient outcomes, practice assessment tools and performance measures relevant to internal medicine.
Resources:
- JAMA, 2023, It Takes an Average of 17 Years for Evidence to Change Practice—the Burgeoning Field of Implementation Science Seeks to Speed Things Up, perspectives on the protracted time it takes to implement practice changes and the role of implementation science.(71)
- National Association of Chronic Disease Directors, Chronic Kidney Disease Detection and Education Program Case Story, overviews outcomes of the CKD Learning Collaborative, an innovative framework designed to facilitate the cross-disciplinary collaboration needed for systems change and successful care transformation in kidney disease.
Ensure care team members executing the CKD intervention helped identify implementation strategies aligned with practice or clinic needs and requirements.
Tools:
- Agency for Healthcare Research and Quality (AHRQ), EvidenceNOW Tools for Change, overviews tools and resources to help primary care practices, practice facilitators and others who support practices, make changes to engage in quality improvement activities.
Resources:
- Agency for Healthcare Research and Quality (AHRQ), Create and Support High Functioning Care Teams to Deliver High-Quality Evidence-Based Care, succinct information on the creation and support of effective care teams that deliver evidence-based, high quality patient care.
Consider implementation of an electronic health record-based CKD registry.
Resources:
- BMC Nephrol, 2019, Development of an electronic health record-based chronic kidney disease registry to promote population health management, overviews CKD registry development and how it can identify modifiable CKD care gaps and enable a population health strategy implementation.(72)
Develop the recommended CKD care plan for your institution.
Resources:
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Development of an Electronic CKD Care Plan, evidence-based suggestions for data elements and standards for building an electronic CKD care plan.
Consider developing CKD clinical decision support.
Resources:
- Pop Hlth Manage, 2021, Redesigning Kidney Disease Care to Improve Value Delivery, examines a machine learning model utilizing electronic health record (EHR) data to improve CKD care in a health system while advancing value.
- J Am Board Fam Med, 2016, Use of Clinical Decision Support to Improve Primary Care Identification and Management of Chronic Kidney Disease (CKD), an early but insightful evaluation of the use of clinical decision support to facilitate improved CKD diagnosis and management.(73)
- Sonic Healthcare USA, Chronic Kidney Disease Population Health, overview of CKD assessment utilizing tools and resources available from a national clinical laboratory.
- LabCorp, Diagnostic Assistant, overview of CKD assessment utilizing tools and resources available from a national clinical laboratory.
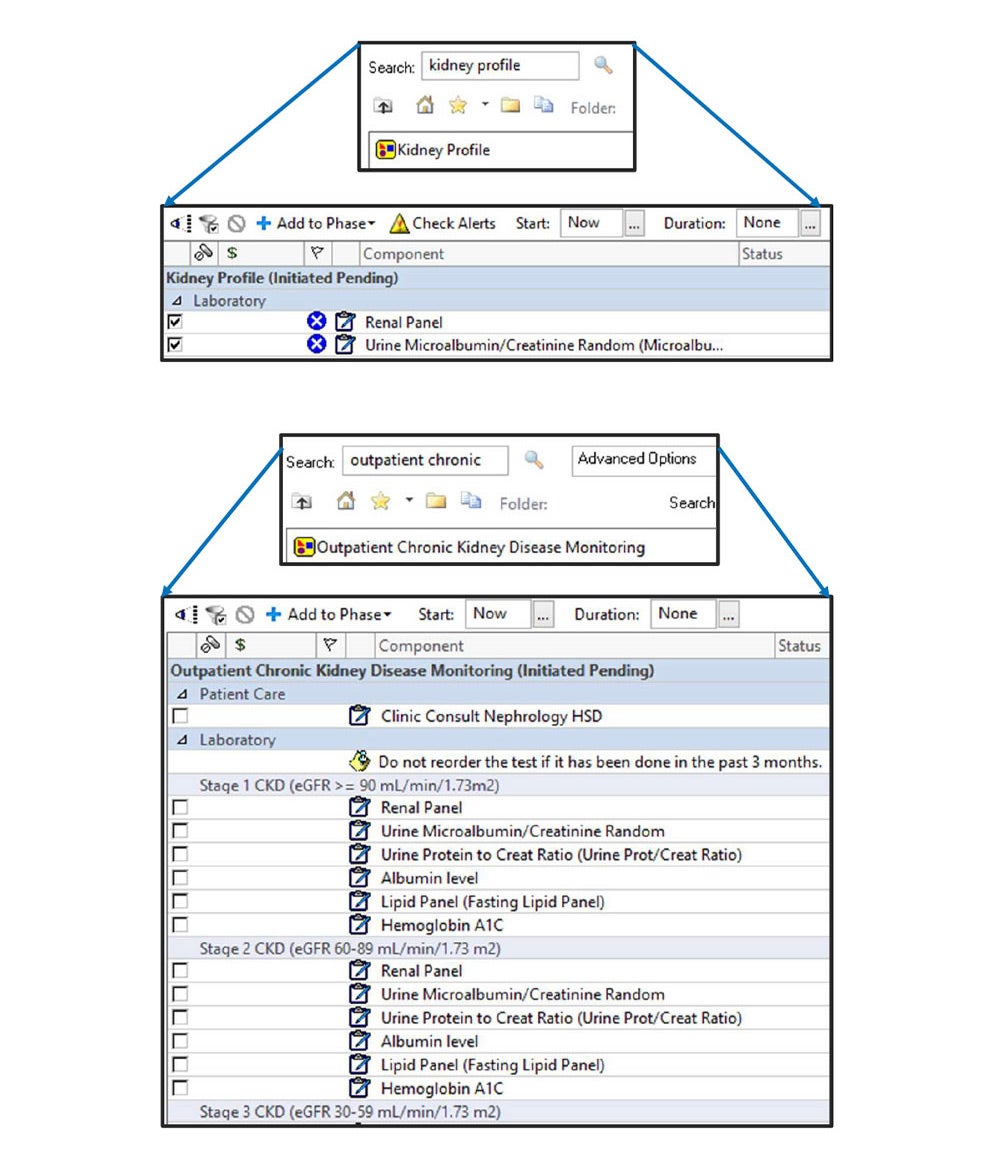
Review / update diabetes and hypertension order sets to include agreed upon CKD parameters including assessment with the Kidney Profile, medication management, referrals.
Tools:
- NKF, Management Algorithm: How to Manage your CKD Patients, an NKF tool that facilitates management of patients with or at risk for CKD
Resources:
- NKF, Closing the Testing Gap by Implementing the Kidney Profile, a virtual meeting of laboratory, IT, data informatics, and quality improvement leaders that highlights successful strategies for implementation, discusses and trouble shoots challenges, and identifies strategies to ensure the Kidney Profile is utilized by clinicians once it is implemented
- Clin J Am Soc Nephrol, 2014, Implementation of a CKD Checklist for Primary Care Providers, evaluation of a CKD checklist (outlining CKD management guidelines) found significant improvement in adherence to management guidelines.(74)
Kidney Profile Order Set Example:
Order sets are adaptable EHR tools that facilitate ordering components of effective clinical care. The order set in the Example has been configured to accommodate institution preferences while still advancing guideline-concordant CKD testing: eGFR (part of the Renal Panel) AND uACR (listed individually with older nomenclature, Urine Microalbumin/Creatinine).
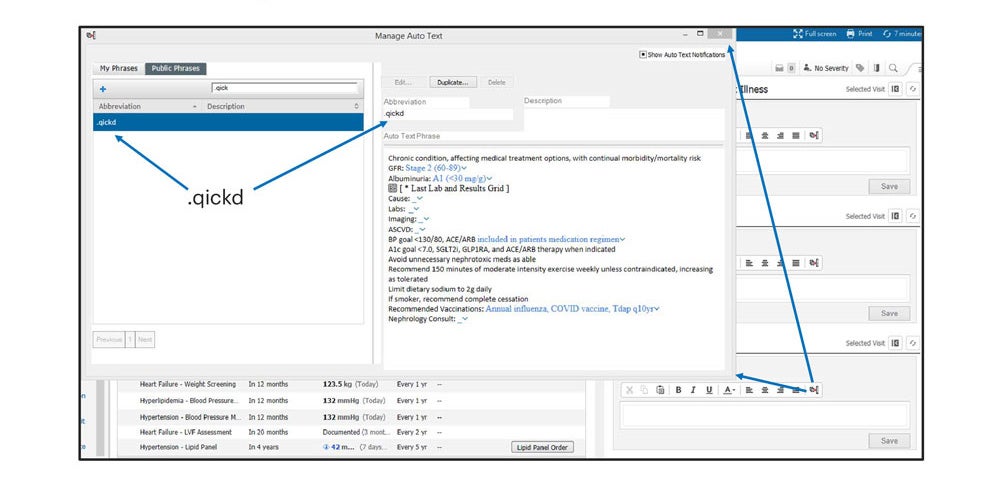
Where appropriate create dot phrases to facilitate entry of CKD information.
Example of Public Dot Phrase for CKD:
When a dot phrase, often an abbreviation or acronym, is typed into the EHR, it triggers pre-saved components of effective care which are dropped into progress notes. The dot phrase example includes components of effective care for Stage 2 CKD.
Consider use of the Kidney Health Evaluation for Patients with Diabetes MIPS measure.
Tools:
- Centers for Medicare and Medicaid Services (CMS), Kidney Health MIPS CMS951v1, details the Kidney Health Merit-based Incentive Payment System (MIPS) clinical quality measure.
Include social determinants of health assessment in the CKD intervention.
Tools:
- Centers for Medicare and Medicaid Services (CMS), The Accountable Health Communities Health-related Social Needs Screening Tool, screening tool to identify and address health-related social needs for Medicare and Medicaid beneficiaries.
- Agency for Healthcare Research and Quality (AHRQ), Identifying and Addressing Social Needs in Primary Care Settings, downloadable resource to help primary care practices identify patients with social needs (e.g. food, housing) and social determinants of health in order to help tailor care to patient circumstances.
- Health Leads, The Health Leads Social Health Data Toolkit, downloadable workbook and toolkit to help healthcare and social health teams collect and apply social health program data.
- American Academy of Family Physicians (AAFP), The EveryONE Project™ Toolkit, Advancing Health Equity through Family Medicine, tools and resources created to promote diversity, address SDOH and advance health equity in all communities with the goal of improving patient health and helping them thrive.
Consider including resources to address identified social determinants of health needs in the intervention tools.
Resources:
- UNITE US, supports cross-sector collaborative solutions among clinicians, payers, government, non-profits and others to improve health and well-being.
- The 211 Network, confidentially connects those in need to expert, caring help in finding food and assistance with expenses for housing, utilities, healthcare, etc.
Within the context of available resources, consider novel community-level approaches for identified needs related to social determinants of health.
Resources:
- Aunt Bertha, zip code directed search for food, health, housing and employment programs
- SAHF: Stewards of Affordable Housing for the Future, advances creation, and preservation of healthy, sustainable, affordable rental homes for patients of limited economic resources
- NeighborWorks America, drives change at the local level for individuals, families and communities through public and private partnerships
- Community Housing Partners, a resource for quality-built, responsibly managed, service-enriched homes for low-income individuals and families across the Southeast and Mid-Atlantic
Outline a seamless communication strategy among patient care team members.
Tools:
- American College of Physicians (ACP), High Value Care Coordination (HVCC) Toolkit, resources to facilitate more effective and patient-centered communication between primary care and subspecialist clinicians
Resources:
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Collaborate with a Registered Dietitian, overviews the role of the Registered Dietitian with extensive knowledge of CKD diet and nutrition in CKD patient care (includes a link to the Academy of Nutrition and Dietetics directory).
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Professional and Continuing Education, a continuing education resource for CKD care team members, including pharmacists, physicians, and registered dietitians.
Make CKD patient education a convenient experience.
Tools:
- NKF, Kidney Basics, various basic CKD patient education resources: Understanding Kidney Health, Risk Factors and Causes, Kidney Health Testing, and Kidney Stones.
- NKF, Patient Education Library: Brochures, a library of patient education brochures that address kidney cancer; hyperkalemia; nutrition; living with kidney disease and kidney failure; kidney failure treatment (ESKD), and kidney disease treatment. (Important information on commercial use and copyright is also provided.)
- NKF, Patient Education (2-Sided Flyers), patient education in a 2-sided flyer format: About CKD; CKD Risk Factors; Diagnostic Tests and Procedures; Diseases and Conditions; Nutrition-General; Nutrition-Superfoods; Living with Kidney Disease and Kidney Failure; Kidney Failure Treatment (ESKD); and Kidney Disease Treatment. (Important information on commercial use and copyright is also provided.)
- Medical Education Institute, Inc., Kidney School, 18 modules of patient education with topics such as living with kidney disease, working with your care team, dialysis, heart health and more.
- NKF, NKF Nutrition Coach, patient-friendly information about the role of nutrition in kidney disease management and overall health, plus general nutrition, appropriate foods, recipes, dietary approaches, and hydration.
Include referral information for local support groups or peer-mentoring programs.
Resources:
- NKF Peers, a peer mentoring program
Utilize multiple channels of outreach to engage patients around CKD awareness and screening.
Tools:
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Family Reunion Kidney Health Guide, suggested opportunities like family reunions to talk with family members about kidney health and the connection between diabetes, high blood pressure, and kidney disease.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Kidney Sundays: A Toolkit, provides a downloadable PDF for health ministry leaders or anyone interested in bringing health programming to their congregation.
Resources:
- Am J Manag Care, 2023, The Role of Faith-Based Models in Community Outreach and Patient Care, summarizes a Cleveland Clinic symposium on collaborations between institutions and faith-based organizations as vehicles to address healthcare disparities and educate underserved communities.(75)
- NC Med J, 2017, From the Memphis Model to the North Carolina Way: Lessons Learned from Emerging Health System and Faith Community Partnerships, reviews health system and congregational partnerships and the collective resources needed to address social determinants of health.(76)
Consider creating a tool kit to address the specific care gap(s) targeted.
Tools:
- National Committee for Quality Assurance (NCQA), Kidney Health Toolkit Improving the Quality of Kidney Care, a resource to help patients and care teams navigate CKD diagnosis, monitoring and management.
- NKF, CKD Toolkits, include educational information and resources for healthcare professionals and the general public.
References
- 71. R. Rubin. It takes an average of 17 years for evidence to change practice-the burgeoning field of implementation science seeks to speed things up. Medical News & Perspectives. JAMA 2023;329(16):1333-1336.
- 72. Mendu ML, Ahmed S, Maron JK et al. Development of an electronic health record-based chronic kidney disease registry to promote population health management. BMC Nephrol 2019 20:72.
- 73. Litvin CB, Hyer M and Ornstein SM. Use of clinical decision support to improve primary care identification and management of chronic kidney disease (CKD). J Am Board Fam Med. 2016 Sep-Oct;29(5):604-12.
- 74. Mendu ML, Schneider LI, Aizer AA et al. Implementation of a CKD checklist for primary care providers. Clin J Am Soc Nephrol. 2014 Sep 5;9(9):1526-35.
- 75. The role of faith-based models in community outreach and patient care. Symposium Recap. Am J Manag Care. April 2023.
- 76. Cutts T, Gunderson G, Carter D et al. From the Memphis model to the North Carolina way: lessons learned from emerging health system and faith community partnerships. NC Med J. 78 (4): 267–72.