Last updated: July 25, 2025
Medically reviewed by: NKF Patient Education Team
C3G, or complement 3 glomerulopathy, is a rare kidney disease with a lifelong impact.
About C3G
C3G is a rare kidney disease caused by a part of the immune system (the complement system) damaging the kidneys. C3G stands for complement 3 glomerulopathy.
- C3: complement 3, a blood protein with a role in immunity and the disease.
- G: glomerulopathy, meaning damage to the glomeruli. Glomeruli are tiny filtering units in the kidney that filter, or remove, wastes from your body.
Signs and symptoms of C3G that relate kidney disease include:
Not all people will have these symptoms the same way. It is important to be aware of the above symptoms. Contact a healthcare professional if you or a family member has these symptoms or notices a sudden change in symptoms.
Causes
C3G is caused when parts of the immune system damage glomeruli, tiny filtering units within the kidneys.
Usually, the immune system protects the body from invaders, like viruses, bacteria, and other germs.
The complement system is part of the immune system. It’s a collection of proteins in the blood that usually helps, or complements, the immune system to fight against harmful germs.
However, in C3G, the complement system becomes more active than usual (or overactive). When this happens, more enzymes are made that break down normal complement proteins such as C3. These breakdown products, or pieces, of C3 are deposited, or gather, in the kidney. This sets off reactions that injure the glomeruli. Damaged glomeruli can't filter the blood very well, and less urine is made. If this continues, more kidney tissue can become damaged, toxins can build up in the blood, and the kidney is less able to do it’s important jobs to keep you healthy.
We’re not always sure why this happens. However, there are several possible reasons. Sometimes it’s related to changes in your genes (variants). In other cases, it may be triggered by certain infections or other immune problems. Whatever the reason, it’s not something you did to yourself.
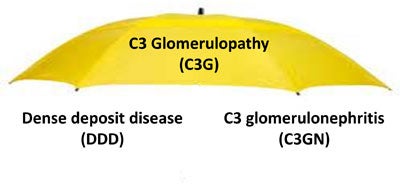
DDD and C3GN can happen at any time and are serious diseases. Both are also treated the same way. However, DDD and C3GN have some differences. They look different under a special microscope called an electron microscope. DDD is seen more often in adults, while DDD is seen more often in children and younger people. Both DDD and C3GN can lead to kidney failure, but C3GN can progress faster.
Before 2013, some people with C3G were given a diagnosis of "membranoproliferative glomerulonephritis (MPGN)" or "mesangioproliferative glomerulonephritis." These same people would now be diagnosed with C3G based on updated definitions of these diseases.
| Names before 2013 | Names after 2013 |
| MPGN 1 or 3 | C3 glomerulonephritis (C3GN) |
| MPGN 2 | Dense deposit disease (DDD) |
Complications
Complications of C3G can include:
- High blood pressure (hypertension)
- High cholesterol
- Gout
- Vision problems (drusen)
- Kidney failure
High blood pressure and kidney disease can also lead to heart problems in C3G.
Diagnosis
A diagnosis can include an observation of any symptoms, blood and urine tests, and a kidney biopsy.
A urinalysis is a test that checks your urine for signs of health issues.
An eGFR, or estimated glomerular filtration rate, is a blood test that shows how well your kidneys are filtering, or removing, wastes form your blood.
A urinary albumin-to-creatinine ratio (UACR) is a urine test that checks for high protein (albumin) in the urine, which is a sign of kidney damage.
A urine protein-to-creatinine ratio (UPCR) may also be used. This test is similar to the UACR test, which measures albumin. Instead of measuring only the amount of albumin in your urine, it measures all the different proteins that may be present. A UPCR level of 150 mg/g or more can be a sign of proteinuria.
A kidney biopsy is required to definitively confirm a C3G diagnosis. A kidney biopsy is a procedure where a tiny piece of your kidney is surgically removed with a special needle, and looked at under special microscopes. The kidney biopsy may show lots of breakdown products of C3, without other proteins, in the glomeruli, which usually means C3G.
To see if the C3G is DDD or C3GN, other portions of the biopsy may be viewed with an electron microscope that can magnify the glomeruli thousands of times. With this method, the exact location of the C3 in the glomeruli can be seen. Depending on where the C3G is located (or its pattern of damage) a diagnosis of DDD or C3GN can be given.
C3G
Sign up for a deep dive into Complement 3 Glomerulopathy (C3G)
Learn about Complement 3 Glomerulopathy (C3G), receive additional resources, and learn so much more.
Treatment
Treatment for C3G includes managing blood pressure, proteinuria, and cholesterol with medications, lifestyle changes, and complement-targeting therapies.
Each of the two types of C3G - DDD, or dense deposit disease, and C3GN, or C3 glomerulonephritis - are treated the same way.
You should talk with a healthcare professional about your condition, because, like many kidney diseases, the progression of C3G is variable and depends on many factors. Some people may live with the disease for years without complications while being monitored. C3G can also lead to kidney failure, which requires a kidney transplant or dialysis to stay alive.
Currently, it is difficult to predict which people will progress to kidney failure and which will not. However, the ability for clinicians and researchers to predict what may happen is improving, but it's not a guarantee. Remember, C3G has a lifelong impact, so it is important to keep up with medical appointments, take your medicines, and stay with the treatment plan as recommended by your healthcare team.
Medications
Medications used to slow the process of kidney damage from C3G may include the following:
ACE inhibitors and ARBs are blood pressure medications used to reduce protein loss and control blood pressure.
Corticosteroids and immunosuppressive drugs are medications used to calm (or suppress) your immune system (to which the complement system belongs) and stop it from attacking the filtering units in the kidney (glomeruli). Immunosuppressive drugs are also used by people who received a kidney transplant. They help lower the body’s natural response to fight the new kidney.
A cholesterol medicine, such as a statin, can be prescribed to help protect your heart.
A healthcare professional may suggest that you undergo plasma exchange (plasmapheresis), a special blood filtering process, to remove harmful antibodies. Plasma exchange involves using a machine to separate plasma (along with the harmful antibodies) from blood and then returning the blood back to the person. A person may receive several treatments over a few weeks. Although plasma exchange has been tried in patients with C3G, there is no proof that it always works.
Complement inhibitors (or complement-targeting therapies) are medicines that can target the complement system. There has been interest in the possibility of drugs that inhibit the complement system can be an effective treatment for C3G.
Eculizumab is a drug known as a monoclonal antibody. This drug can specifically target the complement system and has been used to treat C3G. Rituximab is another monoclonal antibody that has been used to treat C3G. These drugs can slow down the complement system and may help people with C3G. However, they do not always work in people with C3G. They can also have major side effects.
Newer drugs that inhibit the complement system are becoming available to treat C3G. These complement-inhibitors, or complement-targeting therapies, are medicines that target, or calm, the complement system, thus helping to treat a disease like C3G by reducing the damage of C3 to the kidney filters. Some of these medicines are in clinical trials and others may be available. You can discuss available treatments or clinical trials for complement inhibitors with a healthcare professional to find out which may be best for you.
- In March 2025, The FDA approved iptacopan for the treatment of C3G. Iptacopan is a complement factor B inhibitor. This drug works by binding to factor B, which regulates the breakdown of C3. The drug previously received approvals to treat paroxysmal nocturnal hemoglobinuria (PNH) and immunoglobulin A nephropathy (IgAN).
In July 2025, The FDA approved pegcetacoplan the treatment of C3G. Pegcetacoplan is a complement C3 inhibitor. This drug works by binding to and inhibiting C3. This can help regulate the breakdown of C3. This approval also included pegcetacoplan for the treatment of immune-complex membranoproliferative glomerulonephritis (IC-MPGN). IC-MPGN is similar to C3G, but it is a distinct disease. The drug previously received an approval to treat paroxysmal nocturnal hemoglobinuria (PNH).
Nutrition
Practicing a healthy lifestyle and getting regular exercise should also be part of the treatment plan. You may need to limit your sodium, or salt intake, especially if you have high blood pressure. You may also be asked to change your diet in others ways. A dietitian can help with a meal plan that’s right for you.
Preparing for your appointment
Questions to ask
- What was my most recent uPCR or uACR result? If my last result was not at goal, what can I do to make it lower?
- What is my risk of developing kidney failure because of my C3G?
- What lifestyle changes do you suggest I make to help prevent complications?
- Are there any changes I need to make with my diet? Can a dietitian help me with my diet?
- Do I have to make any changes with my medications?
- What symptoms should I watch for that might indicate my condition is worsening?
This video series helps you or your loved ones better learn about the following:
What is C3G? How is C3G diagnosed? How is C3G treated?
In this new research study, share your experience living with kidney disease to improve future kidney care.