Last updated: February 19, 2026
Medically reviewed by: NKF Patient Education Team
In collaboration with:
Glomerular diseases are a group of kidney disorders that damage the glomeruli. Learn about glomerular diseases, including causes, symptoms, diagnosis, and treatment.
Audio Summary of Glomerular Diseases
This audio summary was created with AI, using the National Kidney Foundation content as the exclusive source. NKF clinical experts have reviewed it for accuracy.
About Glomerular Diseases
Glomerular diseases are a group of kidney disorders that damage the tiny filtering units in the kidney (glomeruli).
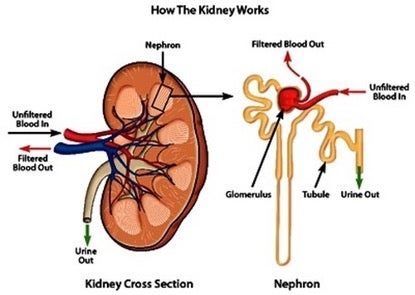
Specifically, glomerular diseases involve damage to glomeruli. Your kidneys may be small, but they perform many vital functions that help maintain your overall health, including filtering waste and excess fluids from your blood. Your kidneys have about one million tiny filter units called nephrons. Each nephron has a glomerulus, so that means there are over one million of them too. More than one glomerulus are called glomeruli. Glomeruli work like strainers used in cooking. While blood moves through them, they let waste and extra water pass into the nephrons to make urine. At the same time, they hold back the protein and blood that your body needs. Many diseases affect kidney function by attacking the glomeruli. When the glomeruli become damaged and cannot do their job, it is called glomerular disease.
There are two main groups of glomerular diseases. Glomerulonephritis happens when the kidneys' blood filters (glomeruli) become inflamed and scarred. Glomerulosclerosis happens when there is damage to the glomeruli caused by hardening and scarring of blood vessels.
Not all people will have these symptoms the same way. Also, a glomerular disease can have other symptoms not listed above. It is important to be aware of these symptoms. Contact a healthcare professional if you or a family member has these symptoms or notices a sudden change in symptoms.
Causes
Glomerular diseases include many conditions with different causes or triggers. It can be caused when parts of the immune system damage glomeruli, tiny filtering units within the kidneys. Usually, the immune system protects the body from invaders, like viruses, bacteria, and other germs. Sometimes, the immune system may become overactive, or may have other problems that lead to kidney damage. There are several possible reasons for this. Sometimes it’s related to changes in your genes (variants). In other cases, it may be triggered by certain infections or other immune problems. Environmental factors can also add to risk. These factors contribute to kidney damage.
Complications
Complications can vary depending on the type of glomerular disease. However, over time, a glomerular disease can stop your kidneys from getting rid of wastes in your blood. When this goes on for a long time, waste builds up in your blood, and you may have chronic kidney disease. This can progress to kidney failure. A glomerular disease can also lead to heart disease, depending on the disease and how advanced it is.
Some people with glomerular disease have nephrotic syndrome (also called nephrosis). Nephrotic syndrome happens when your kidneys lose large amounts of protein in your urine (proteinuria) and causes extra fluids and salt build up in your body. This causes you to have swelling (edema), high blood pressure, and higher levels of cholesterol.
Diagnosis
Generally, a diagnosis can include any combination of symptoms, blood and urine tests, a kidney biopsy, genetic testing, and antibody testing.
A urinalysis is a test that checks your urine for signs of health issues.
An eGFR, or estimated glomerular filtration rate, is a blood test that shows how well your kidneys are filtering, or removing, wastes form your blood.
A urinary albumin-to-creatinine ratio (UACR) is a urine test that checks for high protein (albumin) in the urine, which is a sign of kidney damage.
A urine protein-to-creatinine ratio (UPCR) may also be used. This test is similar to the UACR test, which measures albumin. Instead of measuring only the amount of albumin in your urine, it measures all the different proteins that may be present.
A kidney biopsy is a procedure where a tiny piece of your kidney is surgically removed with a special needle, and looked at under special microscopes. These microscopes reveal patterns of damage that can help identify a disease. In many glomerular diseases, a kidney biopsy is required to definitively confirm a diagnosis of a certain glomerular disease.
Genetic testing may also be used if a disease has a known genetic cause. The test uses a sample of blood or saliva. Samples are sent to a lab, which determines whether they contain to any gene variants, or changes, that have known links to a specific disease. Genetic testing can be ordered by a physician or genetic counselor. A genetic counselor is a healthcare professional with special training in genetics and genetic diseases. They can help answer questions about the test and its results
Antibody (serology) testing may also be used to check for specific proteins (antibodies) your immune system makes to fight infections like viruses or bacteria, or to detect autoimmune conditions. Antibody testing can be used to detect a certain infection, such as flu or COVID. With glomerular disease, an antibody test may be used to detect certain autoantibodies linked with a certain disease.
Treatment
Treatment will depend on the type of glomerular disease you have. Your healthcare team will work with you to create a treatment plan to help prevent kidney disease or keep it from getting worse. Certain nutrition and lifestyle recommendations and medicines may be involved. Most people with glomerular disease will likely need to lower their intake of sodium. Be sure to keep up with medical visits.
Depending on the glomerular disease, ACE inhibitors or ARBs may be used. These are blood pressure medications used to reduce protein loss and control blood pressure. Corticosteroids and immunosuppressive drugs are medications used to calm (or suppress) your immune system and stop it from attacking the filtering units in the kidney (glomeruli). Immunosuppressive drugs are also used by people who received a kidney transplant. They help lower the body’s natural response to fight the new kidney.
Other medications have also become available for certain diseases such as C3G, IgAN, aHUS, and lupus, Check with your healthcare team about new treatments and if they might be right for you.so check with your healthcare team about new treatments and if they might be right for you. New medications for different diseases are being researched, so you can ask your healthcare team if any clinical trials are available and if they might be right for you.
A glomerular disease can also lead to kidney failure, which requires a kidney transplant or dialysis to stay alive.
It is important to pay attention to signs and symptoms and let your healthcare team know as early as possible when you notice them. Treating conditions that can cause glomerular disease may help prevent it from getting worse and slow down the damage to your kidneys.
Preparing for your appointment
Questions to ask
- Am I at risk for a glomerular disease?
- Is my kidney disease considered a glomerular disease?
- What was my most recent uPCR or uACR result? If my last result was not at goal, what can I do to make it lower?
- What is my risk of developing kidney failure because of my glomerular disease?
- What lifestyle changes do you suggest I make to help prevent complications?
- Are there any changes I need to make with my diet? Can a dietitian help me with my diet?
- Do I have to make any changes with my medications?
- What symptoms should I watch for that might indicate my condition is worsening?
















